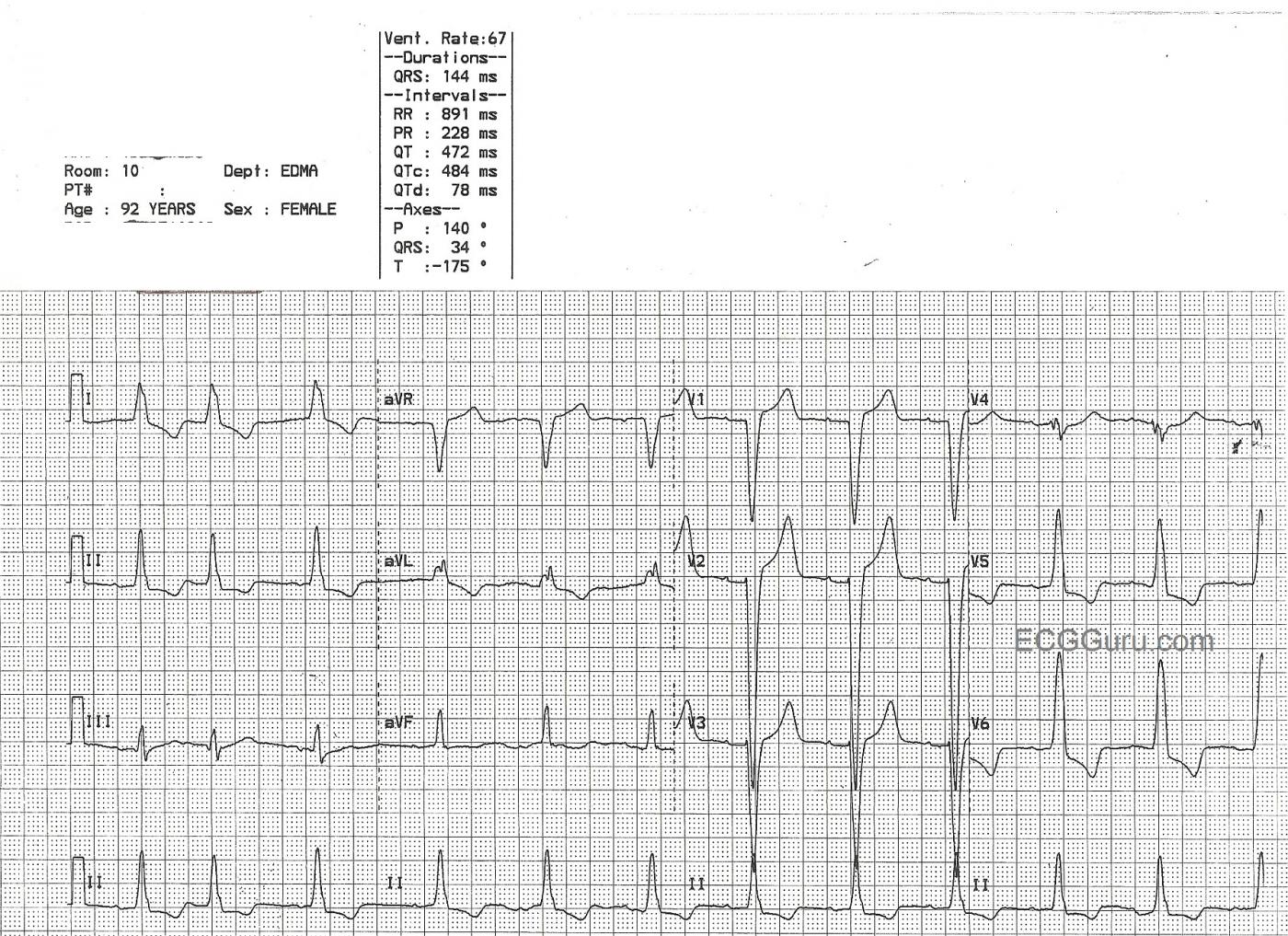
This 92-year-old patient was diagnosed with left bundle branch block on ECG, and left ventricular hypertrophy on echocardiogram. The two conditions are very often seen together, in fact, a majority of LBBB patients have LVH. Since the two conditions can have similar ECG changes, it is difficult from the ECG alone to determine the presence of LVH when LBBB is present. If the ECG criteria for LVH are present, it can be assumed that LVH is present, even in the presence of LBBB. For determining LVH by ECG criteria, the Sokolov-Lyon criteria are commonly used ( S wave in V1 + R wave in V5 or V6 > 35 mm).
The common criteria for left bundle branch block include: wide QRS complex, frontal plane axis normal or leftward, negative QRS in V1, and positive QRS in leads I and V6. LBBB is only found in supraventricular rhythms (not ventricular rhythms). The ST segment and T wave will be negative in leads with positive QRS complexes, and positive in leads with negative QRSs (discordant).
Left ventricular hypertrophy also widens the QRS, although not often as much as LBBB does. There will be discordant ST segments and T waves, which is called the "strain" pattern. It also is easier to diagnose in supraventricular rhythms, because ventricular rhythms usually have large QRS complexes due to the depolarization wave being in one direction across the heart.
For confirmation of LVH, an echocardiogram is recommended.
This ECG also has an interesting rhythm. The first beat appears normal, the second beat is a PAC. The third beat appears to arise from a different focus, which would make it an escape beat, but it is very difficult to determine this due to the very tiny P waves. After a pause, a regular sinus rhythm resumes. To see the P waves, look at the right chest leads: V1, V2, V3. Since left bundle branch block only occurs in SUPRAVENTRICULAR rhythms, it is important to determine the rhythm, and P waves are a definite sign of SV rhythm. We wish the P waves here were taller.
References: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC482258/, http://www.ncbi.nlm.nih.gov/pmc/articles/PMC482000/, http://journal.publications.chestnet.org/article.aspx?articleid=1058580, http://lifeinthefastlane.com/ecg-library/basics/left-ventricular-hypertrophy/
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Complete LBBB plus almost certain LVH
The clinical significance of any conduction block depends upon the company it keeps. Complete RBBB may be seen in patients without any underlying heart disease. In contrast — Complete LBBB Is almost always accompanied by significant underlying heart disease. Statistically — the odds that LVH will be present in a patient who has complete LBBB on ECG approach 80%. This goes up to at least 90% if in addition: i) there are very deep S waves (>25-30mm) in lead(s) V1,V2 or V3 and/or ii) ECG evidence of LAE is also present (ie, wide notched P wave in lead II; deep negative component to the P wave in lead V1).
Ken Grauer, MD www.kg-ekgpress.com [email protected]