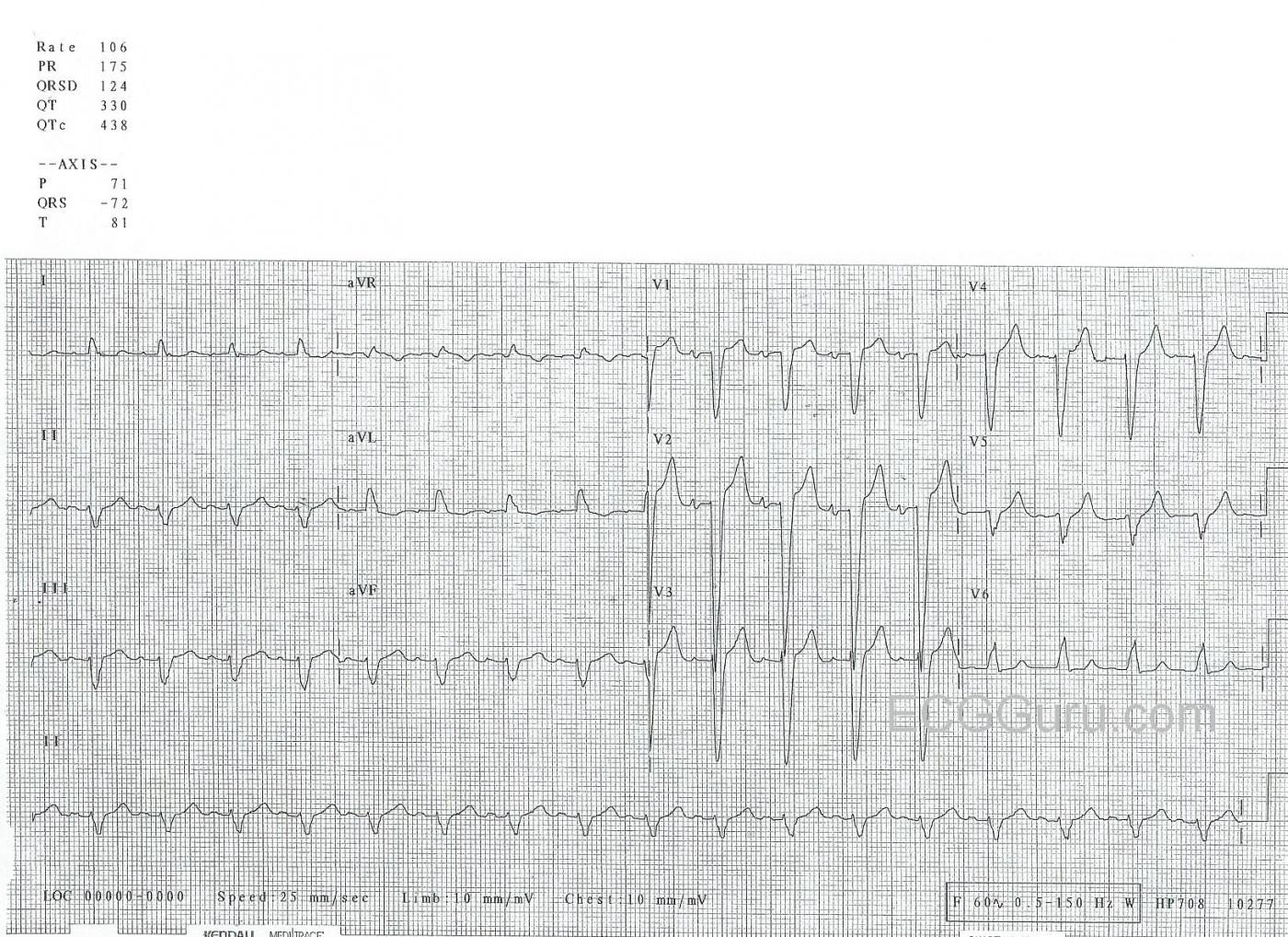
This ECG was taken from an unknown patient. It shows sinus tachycardia with left bundle branch block. The ECG criteria for left bundle branch block are:
* Wide QRS (.12 seconds or greater)
* Negative QRS deflection in V1
* Positive QRS in Leads I and V6
* Supraventricular rhythm
In addition to these criteria, left bundle branch block will cause repolarization abnormalities. This is because depolarization is altered through the left ventricle, which causes repolarization to also be altered. Instead of the electrical impulse traveling down the left bundle branch to depolarize the left ventricle, it depolarizes the right ventricle first, then spreads cell-to-cell across the larger left ventricle. The ST and T wave changes caused by left bundle branch block are normally “discordant”. That is, the ST segment will be elevated in leads with negative QRS complexes, and depressed in leads with positive QRS complexes. This elevation and depression of the ST segment may “imitate” the changes caused by acute myocardial infarction. They may also work to conceal M.I. changes, as we may not recognize STEMI as we attribute the ST changes to the left bundle branch block itself.
For more on determining the presence of acute M.I. when the patient has left bundle branch block, check out these links: ECG Guru, LBBB with AMI; Life in the Fast Lane, Sgarbossa Criteria; EMS 12-Lead, Sgarbossa Criteria; Dr. Smith's Modified Sgarbossa Criteria.
This ECG has another interesting teaching point. In some leads, part of the QRS is flat or nearly flat with the baseline. Look at Lead I for an example. It is very hard to tell that this represents a wide QRS. Fortunately, the precordial leads, especially V1 through V4, show the width better. In reality, all the QRS complexes represent the time it takes to depolarize the ventricles, and that time is the same, regardless of which lead you are looking in. Some leads are just easier than others. It often helps to look at the QRSD (QRS duration) at the top of the page to see how the computer measured the QRS duration. It is usually accurate. In the illustrated case, the QRSD is measured in milliseconds, 124 ms (or .124 seconds).
You might also notice that the frontal plane axis is shifted to the left. That is, Lead II (viewpoint from left leg) has a negative QRS while Leads I and aVL (from left arm) are positive. This is common in left bundle branch block, because the left ventricle is being depolarized from the right ventricle, which is located inferior and medial. Because axis is affected by many factors, left axis deviation is not a prerequisite for the diagnosis of left bundle branch block.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
The Basics of BBB
The case this week is on the ECG diagnosis of complete LBBB. While I essentially agree with Dawn’s description — I’ll offer a slightly different approach that I have used for the past 3+ decades with great success — and which allows me to teach others how to accurately diagnosis RBBB, LBBB and IVCD within seconds — as well as when to suspect that in addition to the conduction defect, there may also be ongoing ischemia infarction. My approach is summarized in an easy-to-follow 17-minute ECG video on, "The Basics of BBB" — See www.bbbecg.com —
The reason we can simplify ECG diagnosis of typical RBBB or typical LBBB — is that you ONLY need 3 leads to make the diagnosis. So while I always look at ALL 12-leads on every tracing — only the “3 KEY Leads” ( = leads I, V1 and V6 ) are needed to diagnosis the BBBs. That is, we need 2 left-sided leads (I, V6) and one right-sided lead (V1). While left-sided leads aVL and V5 often look like lead I, and while right-sided leads V2,V3 often look like V1 — you do NOT need these other leads to make the diagnosis of typical BBB.
As to ST-T waves — while true that in general ST-T waves are “opposite” the predominant direction of the QRS — this is NOT always true in all leads. But it IS true that the ST-T wave in the 3 KEY Leads should always be oppositely directed to the LAST QRS deflection in these 3 Key leads if the ONLY thing operative is the bundle branch block. If either the ST segment or T wave is not directed opposite to the last QRS deflection in each of these 3 key leads — then “something else” (ie, ischemia, infarction) may be ongoing.
While the above sounds complex — seeing what I am describing MAKES THIS SIMPLE. Rather than rewriting the Bundle Branch Block chapter in my book here — I will simply suggest you view my 17-minute video on the Basics of BBB — and my bet is that you’ll find my approach enables accurate determination of whether there is typical RBBB, LBBB or IVCD with or without likely ischemia or infarction in less than 5 seconds for almost any conduction block tracing you are confronted with.
For those who would like my full description — CLICK HERE to download the full chapter on BBB from my book. The part on diagnosis MI with BBB begins in Section 05.24.
-------------
P.S. The ECG in this case shows some subtle abnormalities. While these may or may not be of clinical significance — they should be noted. While QRS morphology of the widened complex is consistent with LBBB (ie, monophasic upright in key leads I and V6; and predominantly negative in V1) — and while the last QRS deflection in lead V1 is opposite the negative QS in V1 — the small-but-upright T wave in both leads I and V6 is not as should be expected for typical LBBB. Instead, the ST-T wave in these lateral leads should be negative. This could reflect ischemia (or even infarction), especially if this ECG finding is new and the patient is having chest pain. Clinical correlation is needed …. The very deep anterior S waves (over 30 mm deep in V2) together with the deep negative component to the P wave in lead V1 suggest in addition to LBBB that there is LVH. And finally — there may be an ever-so-tiny initial q wave in lead aVL. With typical LBBB, there are NO Q waves in leads I, aVL or V6 — so this suggestion of a small q wave in lead aVL might reflect prior scar (infarction).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Quirks and Idiosyncrasies of LBBB
Dawn...
I really don't have much to add to two excellent analyses but I'm not totally without words...
There is a tiny, tiny q wave in aVL - one so small that I wouldn't fault anyone for missing it. I always teach my students that any miniscule "blip" that occurs regulary in the same place is being caused by something that needs to be addressed. One can occasionally see a non-pathological q in aVL during complete LBBB depending on the orientation of the heart in the chest. The initial impulse gets oriented just past +60 degrees and the q wave appears. Seeing one is not exactly like spotting a Sasquatch; you will encounter them from time to time.
The other observation is that this is a complete LBBB with an anterior fascicular block! A lot of people would say "How can you have a left anterior fascicular block (or hemiblock) when there is already a complete LBBB? There are two ways to get an anterior fascicular block: either 1) the anterior fascicle is indeed blocked or 2) nothing is wrong with the anterior fascicle but the posterior fascicle gets activated first.
During normal conduction or during RBBB, the septum is activated from left-to-right about midway between base and apex (sometimes a little bit lower). That is due to the presence of fibers from the septal fascicle or the posterior fascicle. However, with LBBB, the septal activation doesn't begin until the right bundle branch has reached the lower right septal mass in the area of the right anterior papillary muscle (remember: all three fascicles are racing to activate their respective papillary muscles before the rest of the myocardium). Activation then starts in a right-to-left direction near the apex and travels up the septum to the base by cell-to-cell conduction (it has to be cell-to-cell because the right bundle branch is now refractory and there are no pathways traveling within the septum). At that point it re-enters the Purkinje fibers of the left ventricle below the block - either the main left bundle branch or one of the fascicles (and almost always the posterior fascicle). If it enters the posterior fascicle first, the ECG will have the appearance of an anterior fascicular block even though there may be no delay in the anterior fascicle at all. However, if there was a previous anterior fascicular block, it will continue to be manifested on the ECG tracing.
Thanks for the opportunity to comment.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd