This is an interesting case for your students who want to delve into dysrhythmias with an eye on detail. It is also a good teaching case for discussing treatment options when the diagnosis may be uncertain or controversial. I will start the discussion by admitting that I am not an expert of electrophysiology or complex dysrhythmias. My approach has always been more clinical - how is this rhythm affecting the patient and what are the chances it will deteriorate? I hope some of our dysrhythmia Gurus will delve into the rhythm and maybe even provide laddergrams.
The patient: This is a man in his seventies who complains of light-headedness for several days, and feeling worse today, prompting an emergency call. He offers no cardiac history. BP 116/62 and 116/58. Blood glucose 220 mg/dL. Physical exam unremarkable.
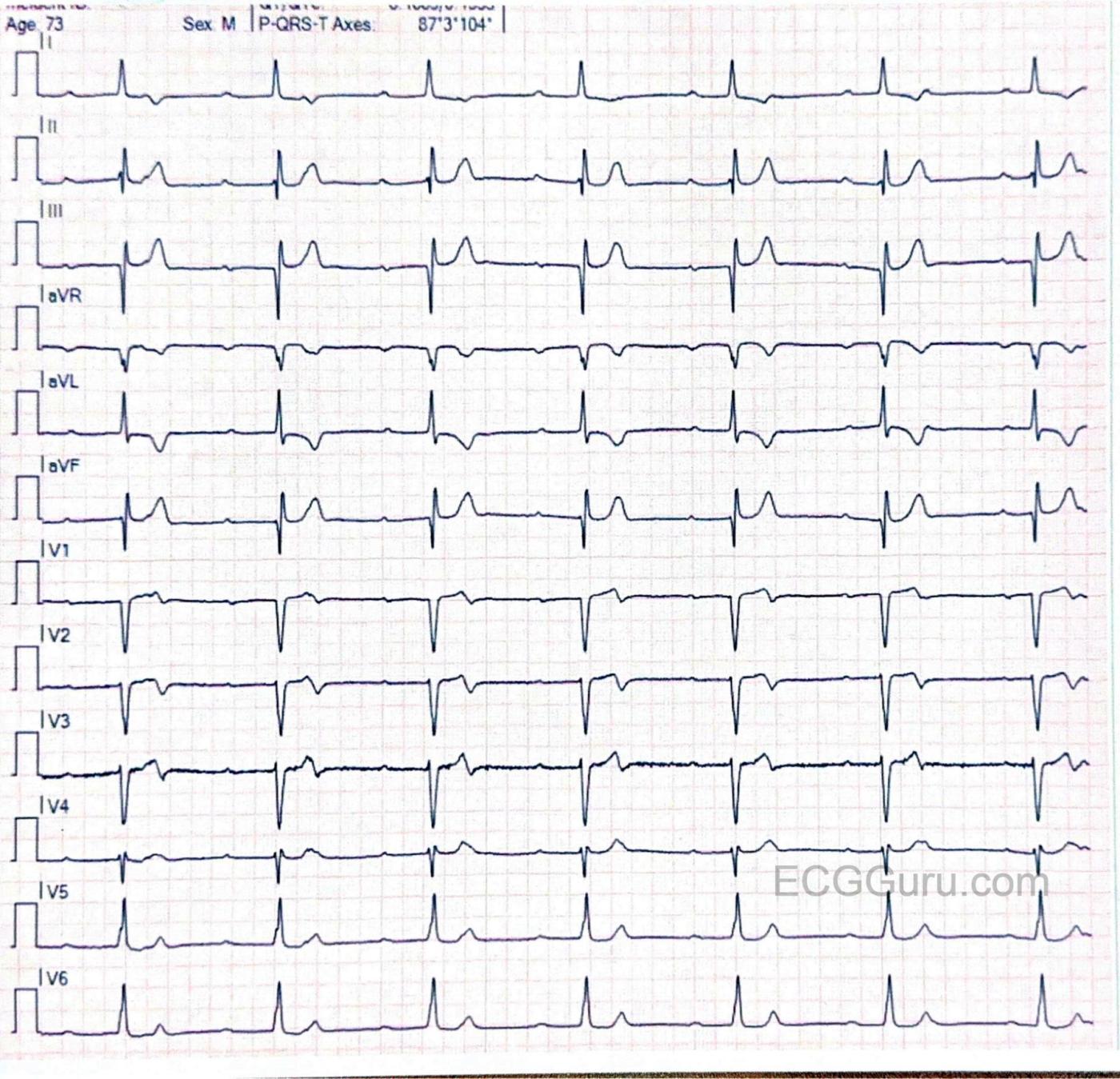
12-Lead ECG : I will admit that, on first quick glance, I thought I was looking at a 2:1 AV block. But on closer inspection, I noted that the "PR intervals" varied, becoming shorter as the strip progressed. Another 12-lead on the same patient showed even more pronounced variations. The atrial rate is about 76 bpm (measured with a digital caliper). The atrial rhythm is fairly regular (allowing for slight variations in sinus rhythm). The ventricular rate is around 39 bpm, almost exactly half that of the atrial rate. This rhythm is also regular. Because of the PRI interval changes, I believe this is complete AVB with an escape rhythm that is just about half the atrial rate. If that is correct, the ventricular rhythm originates in the AV junction, because the QRS complexes are narrow, and the rate is very near 40 bpm. The frontal plane axis is slightly leftward, within normal range, and the R wave progression in the chest leads shows a late transition, with patholoogical Q waves in V1. There are also Q waves in III and aVF.
There are ST and T wave changes in Leads I, aVL, V1, V2, and V3. I do not know if this patient has a history of cardiac disease or a recent complaint of chest pain, but T wave inversion and some biphasic T waves makes me think of reperfusion changes, reflecting a recent M.I. The ST segments in leads with T wave changes are also uncomfortably straight. We do not have followup on this patient's hospital course or treatment.
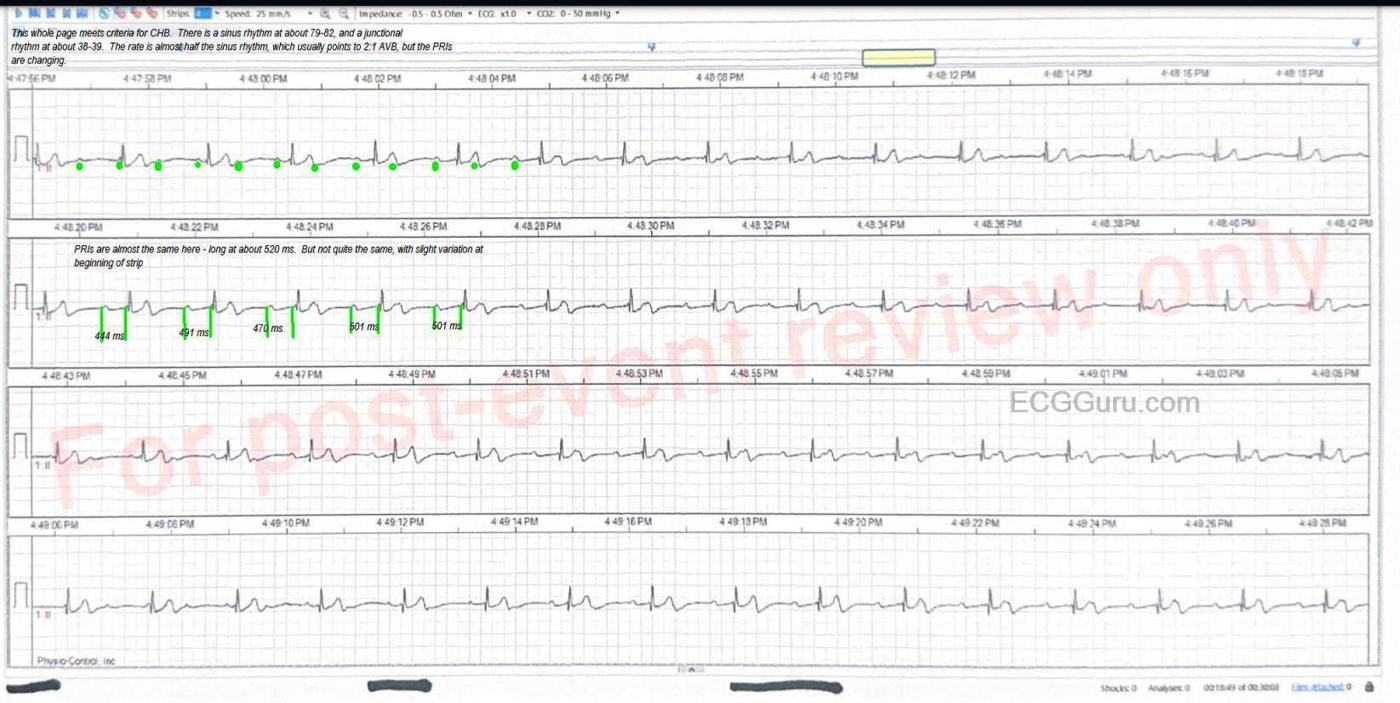
I have included a rhythm strip with some markup for those who would like to really get into the mechanism of this rhythm. For myself, as a retired ER RN and paramedic, I think of the clinical ramifications of such a rhythm.
1) Is this rhythm the result of OMI? This would demand further investigation, probably with a temporary transvenous pacemaker as a safeguard measure.
2) Is the patient tolerating the rate? If not, early transcutaneous or temporary TV pacing would be indicated. The nervous system has signalled the sinus node to produce a rate of around 76 bpm. Because of either CHB or 2:1 AVB, the ventricular rate is about half of that. While the BP seems to be low-normal, we don't know the patient's baseline normal. We don't have any other information about perfusion status, but lightheadedness could be a symptom of poor brain perfusion. I would love to know his skin appearance and temp. We do know he was conscious and alert.
3) The medical providers who must diagnose this rhythm will hopefully assess for OMI, address the rate, and further establish how much AV block is present and where the block is located. Emergency medical professionals should focus on getting the patient to a hospital with cardiac facilities with an optimal rate and the best perfusion possible. Obtaining a good past medical history and medication list would also be a priority, in case the patient loses his ability to communicate.
I welcome a robust discussion about this rhythm and treatment considerations.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
AV Block: What Kind? and Why?
As per Dawn — today's presentation is an excellent teaching case that reminds me of similar cases I saw over the years as overseeing faculty at our Family Medicine Residency Program. The patient is older — and presents with lightheadedness for several days, but no chest pain. His blood pressure is on the low side — and his ECG is some variation of the tracings I would see in others with similar clinical presentations.
First, the history. Lack of chest pain does not rule out a recent cardiac event. The Framingham studies taught us that up to 1/3 of all MIs may not have chest pain. About half of that 1/3 have "something else" — of which dizziness is one definite possibility. The other half of that 1/3 have no symptoms at all — but on follow-up ECGs, definite evidence of an unperceived infarction is seen. The fact that today's case features a several day history of this patient's symptoms means that if an acute cardiac event did occur at the time this patient began having symptoms — ECG changes may be subtle (or perhaps not even present) — and even if serum Troponin values are obtained, they may by this time be normal. Brief — it may not be easy to document that a "silent" MI that occurred days earlier may be the cause of the rhythm disorder.
I will focus on today's 12-lead ECG. The format of this ECG is such that we simultaneousy see the same 7 beats of this 10-second recording in all 12 leads. The QRS complex is narrow with a strictly constant R-R interval consistent with a ventricular rate in the low 40s. As per Dawn — P waves are present, but with a variable PR interval.
PEARL #1 — Among the most common oversights I see even experienced interpreters commit — is the failure to spend 2-to-3 seconds looking in front of each QRS complex in the lead II rhythm strip to verify that there is a P wave, and that the PR interval in front of each QRS remains constant. If the PR interval is not constant — then we do not have a simple sinus rhythm. In today's case — it is easiest to establish that the PR interval does not remain constant by looking at the PR interval of the 1st beat — and comparing this with the PR interval of the last beat. Once you are "clued in" to this difference in PR interval between the 1st and last beats — it becomes much easier to appreciate that the PR interval is actually continually changing.
PEARL #2 — Unless you use calipers, you will never get good at interpreting complex arrhythmias. It does not matter if you are a 1st-year medical student or an experienced cardiologist. You WILL miss subtle-but-important findings if you do not use calipers. The "good news" — is that it takes no more than seconds using calipers to verify that the PR interval varies for each of the 7 beats in this tracing. Making a habit to use calipers for complex rhythms (when the patient in front of you is not "crashing") — will instantly make you a MUCH better interpreter (and you WILL pick up findings that your friendly cardiologist who does not use calipers misses). Best thing — with a tiny bit of practice, your speed interpreting arrhythmias (as well as your accuracy) will dramatically improve when you use calipers.
PEARL #3 — This variable PR interval in today's tracing should immediately suggest that there may be more P waves than just the one in front of each QRS. If so — setting your calipers to HALF the R-R interval will immediately tell you where to look for an extra P wave (if in fact there are 2 P waves for each QRS) — with this "ideal hiding place" being contained within the preceding ST-T wave.
PEARL #4 — Look at the ST-T waves in all 12 leads to see if there is a subtle, ongoing change in morphology. In today's case — I thought lead I illustrates this principle in excellent fashion. As you look at the ST-T wave for each of the 7 beats in lead I — Don't YOU see a slight-but-real change in the ST-T wave from one beat to the next? And if you place your calipers on these changing subtle deformities — we can "march out" a regular P wave rhythm, because there are 2 P waves for each QRS.
PEARL #5 — It is common with 2nd- and 3rd-degree AV blocks for there to be an underlying "ventriculophasic" sinus arrhythmia. Awareness of this very common slight variation in the P-P interval explains why the P-P interval of the extra P waves in today's tracing is not precisely regular.
PEARL #6 — By far, the BEST clue that there is some conduction of P waves in a complex rhythm like this one, is if the R-R interval unexpectedly shortens (ie, shortening of the R-R interval is a "give-away" that one or more P waves are conducting). But there is NO shortening of the R-R interval in both of today's tracing. Therefore — NONE of the many P waves in today's tracing are conducting, despite the very slow ventricular rate that provides more than adequate opportunity for P waves to "have a chance" to conduct. Therefore — today's rhythm is complete ( = 3rd-degree) AV block. The reason for the narrow QRS and slow ventricular rate — is that the escape focus is arising from either the AV node or the Bunlde of His.
PEARL #7 — We now need to correlate today's history with this 12-lead ECG that shows complete AV block. The Q waves in leads III and aVF are deep — and might reflect recent inferior MI. In addition — I thought the T waves in each of the inferior leads are taller and more peaked than is normally expected. And we KNOW the ST coving and fairly deep T wave inversion in lead aVL is not normal — but instead is consistent with a reciprocal change. And, in the chest leads — there is very poor R wave progression until lead V5, as well as biphasic T waves in leads V1-through-V3. In short, while I'm not sure whether we are dealing with inferior or anterior infarction of uncertain age (or perhaps a patient with multi-vessel disease) — the history tells us that there very possibly has been RCA or LAD occlusion as the precipitating event of this patient's complete AV block.
BOTTOM LINE: This man in his 70s is symptomatic from complete AV block with a resultant slow ventricular escape rate.He should be admitted for standard lab, serial Troponins and ECGs — and probably cardiac catheterization to see if there is anything "fixable". If his slow AV block persists — permanent pacing will probably be needed..
Ken Grauer, MD www.kg-ekgpress.com [email protected]