The Patient: Unfortunately, this is an old tracing, and we do not have patient information, other than the list of medications the patient has been taking, (Lasix, Capoten, Ntg, and Procardia). Lasix (furosemide) is a potassium – wasting diuretic. Capoten (captopril) is an ACE inhibitor. Ntg is presumably sublingual nitroglycerine used for angina. Procardia (nifedipine) is a calcium-channel blocker. So, we can assume the patient was probably being treated for angina, heart failure, and hypertension.
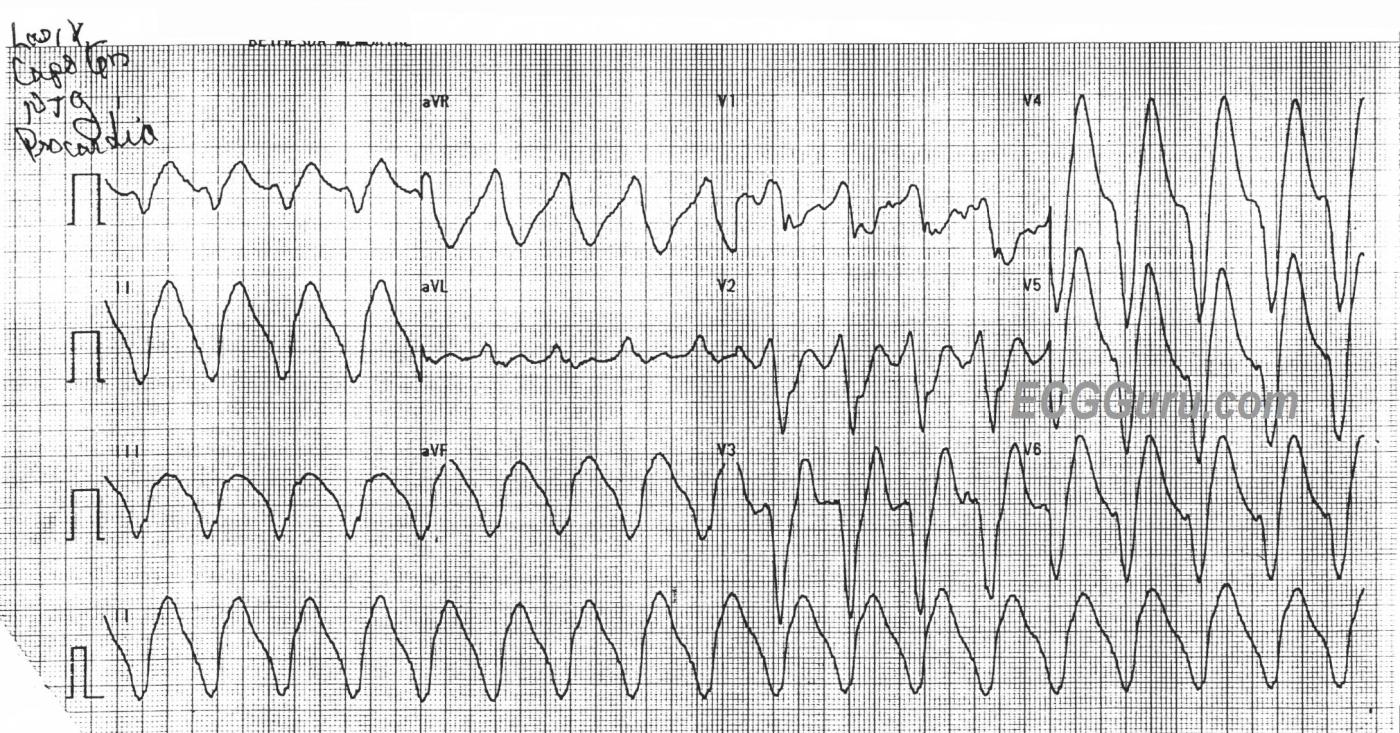
The ECG: The first impression is that is a regular WIDE COMPLEX TACHYCARDIA. The ventricular rate is 100 bpm (Starts a little faster at the beginning at 106, then is 100 by the end). The QRS duration is about 250 ms (.25 seconds) – VERY WIDE. There appear to be P waves outside the QRS complexes in V1 and aVL, but probably buried in the ST-T of other leads.
We were all taught to treat all wide complex tachycardia (WCT) as VENTRICULAR TACHYCARDIA (VT) until proven otherwise. This is a very good rule, especially in an emergency setting. It pays to take a moment to consider the possibility of REGULAR REALLY WIDE COMPLEX TACHYCARDIA (RRWCT) before making a treatment decision.
An extremely wide QRS can occur because of a number of very concerning reasons, most involving blockade of the sodium channels. Included in this category are:
· Hyperkalemia. (effectively blocks the Na channels)
· Overdose of sodium-channel blocking drugs
· Acidosis of toxicity and sepsis
If a wide-complex rhythm is over 100 bpm, we call it “tachycardia”, but it is not necessarily “ventricular”.
The biggest danger for the patient is that we might call this rhythm VT and choose a sodium-channel blocker antiarrhythmic drug to treat it, such as amiodarone, lidocaine, or procainamide.
This could kill a patient who doesn’t have VT, but instead has RRWCT.
So, what features of this ECG suggest RRWCT?
· The QRS is VERY wide at .25 seconds. VT is usually LESS than 200 ms wide.
· The rate is 100 bpm. VT is usually at least 120 bpm.
· There may be P waves associated with the QRSs, but this may be hard to be sure of in an emergency setting.
Normally, the patient presentation is likely to give us a clue as to the origin of the WCT. Preexisting sepsis, drug overdose, cocaine use, or renal failure make consideration of RRWCT a must. Acute chest pain is much more suggestive of VT. In the setting of RRWCT, think TOXICITY or METABOLIC causes.
We usually avoid commenting on treatment options in the initial ECG interpretation comments, as our readers work in different settings with different treatment options available. But, it bears mentioning that the initial treatment for RRWCT is calcium and sodium bicarbonate. This choice will not harm the patient who actually has VT, so it is often worth trying if the rhythm is suspected of being RRWCT. Many EMS agencies in the U.S.A. have protocols for this treatment, either labeled for RRWCT or for hyperkalemia. We are including here some references for those who would like to know more.
NIH, National Library of Medicine. Stat Pearls (internet). Wide QRS Complex Tachycardia. June, 2023.
Hippo EM, Dr. Amal Mattu, How do you avoid a clean kill with wide complex tachycardia?
You Tube Video, 2017.
https://www.youtube.com/watch?v=UXh8PS9dtmo
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Really Wide Regular WCT (HyperK)
Dawn's presentation says it all for today's case — namely a "Really" Wide Regular WCT ( = Wide-Complex Tachycardia) rhythm without clear sign of sinus P waves at a rate of ~105/minute. As per Dawn — the modest ventricular rate — bizarre QRS morphology — and the especially markedly prolonged QRS duration all suggest some type of toxicity rather an ischemic ventricular tachycardia.
With full realization that tall peaked T waves may be seen with ischemic VT — the giant peaked T waves in leads V3-thru-V6 (more than 20 mm tall in lead V4 — which is a greater amplitude than depth of the S wave in this lead) — strongly suggest hyperkalemia.
Finally, although we lack lab results — inclusion of an ACE-inhibitor among this patient's list of medications clearly predisposes to hyperkalemia.
Bottom Line: I would be surprised if serum K+ was not significantly elevated. I would immediately treat with one or more doses of IV Calcium — and expect prompt improvement in the ECG appearance.
For more on various aspects of the ECG diagnosis and empiric treatment of hyperkalemia — Please check out my ECG Blog #275 (https://tinyurl.com/KG-Blog-275 ).
Ken Grauer, MD www.kg-ekgpress.com [email protected]