The Patient: Sixty-year-old man with a complaint of severe substernal chest pain. Denies hx of M.I., but reports feeling short of breath on exertion for about a year. Hx of hypertension, but admits he is non-compliant with his medication. Appears pale and diaphoretic, BP 110/68.
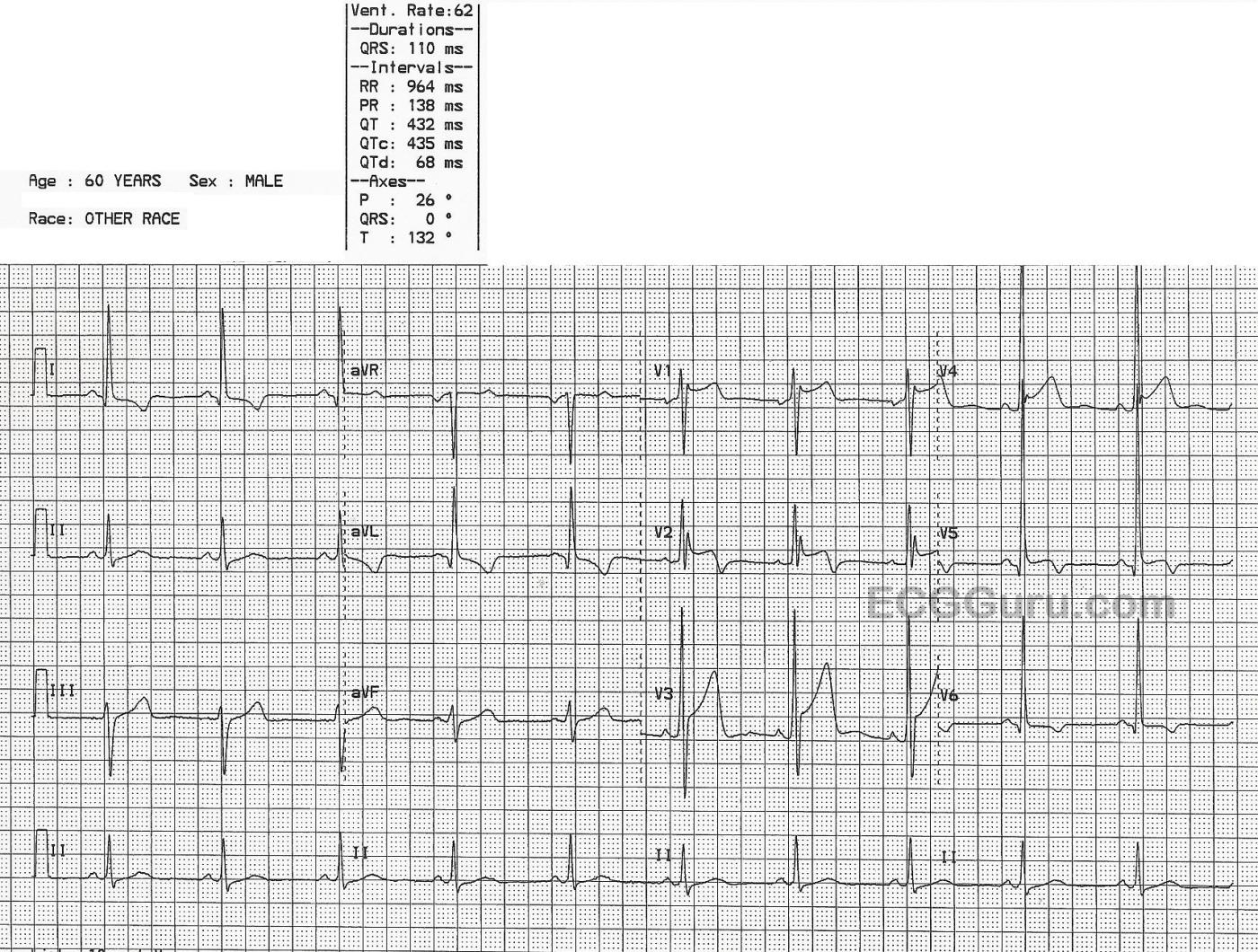
The ECG: The rhythm is sinus at 62 bpm. The QRS is slightly wide at 110 ms (.11 seconds), but still within normal limits. The intervals are WNL. The frontal plane axis is slightly leftward, while still normal. The QRS complexes are tall, especially on the left side. The voltage meets criteria for left ventricular hypertrophy (LVH). This is also called left ventricular enlargement (LVE). There are several accepted criteria for determining LVH, and this ECG meets them all. The V1 S wave plus the V5 R wave equal 52 or 52 mm. There is a slightly increased R wave peak time in V5 and V6 (normal is about one small block). There is ST depression and T wave inversion in the lateral leads: I, aVL, V6. This is called the "strain" pattern. V5 is also a lateral lead, but something else is preventing ST depression.
Note the ST elevation in V1 through V5. This is acute transmural ischemia, or ST elevation M.I. The STE in V5 was enough to overcome the STD caused by the LVH. The more modern term for these ECG changes is “OMI”, or occlusion myocardial infarction . https://litfl.com/omi-replacing-the-stemi-misnomer/ This term replaces "STEMI", as it includes myocarial injury with ST elevation and also with other ECG findings that are classified as "STEMI Equivalents".
We don't have information regarding the patient's outcome, but it is worth mentioning that the BP of 110/68 is probably low for him, and he has poor peripheral perfusion, evidenced by his pale skin and sweating.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
What is the REAL diagnosis?
I found today's tracing of special interest — because it evokes a series of ECG diagnoses — each of which may complicate diagnosis of the other entities — and all of which leave me with more questions than answers.
The history is relevant. The patient is a 60-year old man with a history of hypertension. He presents with new severe CP (Chest Pain) — and he appears pale and diaphoretic with a low BP for a hypertensive patient ( = 110/68 mm Hg). Given this worrisome history — regardless of whether the ECG does or does not look acute — we need to be of the mindset that acute OMI ( = Occlusion-based Myocardial Infarction) is the diagnosis UNTIL we can prove otherwise. That said — Is this REALLY an acute STEMI?
The rhythm is sinus at 60/minue. All intervals (PR, QRS, QTc) look normal. The frontal plane axis is slightly leftward (at about -15 degrees) — but not leftward enough to qualify as LAHB.
There is definite LVH — with marked increase in QRS amplitude and ST-T wave changes in leads I and aVL (if not also V6) consistent with LV "strain". This increase in QRS amplitude is extreme (ie, R = 15 mm in lead I; 23 mm in lead V6; and 39 mm in lead V5 — as well as most probably being responsible for the literally "off the page" R wave positivity in lead V4). The importance of recognizing how extreme this increase in QRS amplitude is — is that it influences our ability to appreciate the presence and meaning of ST-T wave changes. It also makes me curious to search for a recent Echo on this 60yo man with "hypertension" — as I would not be at all surprised to find an underlying cardiomyopathy that further affects our ability to determine from a single ECG whether or not there is suggestion of an acute MI with need for catheterization.
Looking elsewhere in the chest leads — there is an unusual RSr' complex in leads V1,V2 of uncertain significance in both leads V1 and V2. Lack of terminal S waves in any of the lateral leads question whether this indicates some form of rbbb conduction OR is simply fragmentation from some underlying cardiomyopathy.
The "saddleback" ST elevation shape with terminal T wave positivity in lead V1 looks more to me like a Brugada-1 ECG pattern than like the ST elevation of a new, acute STEMI (See my attached illustration).
I believe there is a prominent J-point notch at the onset of the slightly elevated, and concave-upsloping ST segment in lead V4. Overalp of huge R waves in neighboring leads make it difficult to appreciate this notch — but, given how often such notching is seen with repolarization variants — I wonder if the concave-up ST elevation with terminal T inversion in lead V5 is simply a "transition" lead between a longterm early repolarization variant and marked LVH ( = the picture that we may be seeing between lead V4 and V6).
The above said — the most concerning lead to me is lead V3, in which the amount of J-point ST elevation is no less than 6 mm! That said — this is associated with another concave-up ("smiley"-configuration) ST segment and the unusual appearance of a huge R wave in lead V3 ( = 27 mm) that is rarely seen so soon in R wave progression. Could this also be a reflection of marked LVH together with some extreme repolarization variant —and/or — some longstanding ECG changes from hypertensive cardiomyopathy — and/or possible prior events? — and/or all of the above with a new STEMI superimposed?
Which leaves us with the potentially worrisome ST-T wave appearance in lead V2 — OR — does the QRST appearance in lead V2 simply represent another "transition lead" between the Brugada-1 pattern in lead V1 (which may or may not have clinical relevance) — the RSr' morphology of uncertain etiology — longstanding J-point ST elevation from a repolarization variant — OR — worrisome ST elevation from an ongoing acute event in this 60yo man with new CP?
My "bottom line" — is that I simply do NOT know the answer. I'd LOVE to know follow-up of this case, but unfortunately there is none. That said — I think it a GREAT case for discussion, because to me it challenges readers to see how many of the above considerations that I mentioned were noted — and WHAT THE READER WOULD DO if presented with this single ECG in a 60yo man with new CP?
My answer — is that I would NOT activate the cath lab based on this single tracing. I suspect this ECG does not represent an acute STEMI — but the "onus of proof" is on me as the provider to confirm that impression WITHIN a FEW quick minutes. Finding a previous ECG would be invaluable! The evolution of acute ST-T wave changes during an ongoing acute STEMI is often rapid — so I'd repeat this initial ECG within no more 10-15 minutes. We need to be bedside to verify the history — recheck BP — determine if other reasons for a low BP might be present (ie, hypovolemia?) — and of course, as soon as stat Troponins return (and hopefully BEFORE this) — an answer should be forthcoming.
I'd love to find out what happened ...
P.S. For a similar case regarding discussion of "Acute or Not Acute?" — Please check out the November 17, 2024 post in Dr. Smith's ECG Blog — this post by Dr. Willy Frick, with My Comment that I write at the bottom of the page — GO TO: https://hqmeded-ecg.blogspot.com/2024/11/acute-chest-pain-and-abnormal-e... —
Ken Grauer, MD www.kg-ekgpress.com [email protected]