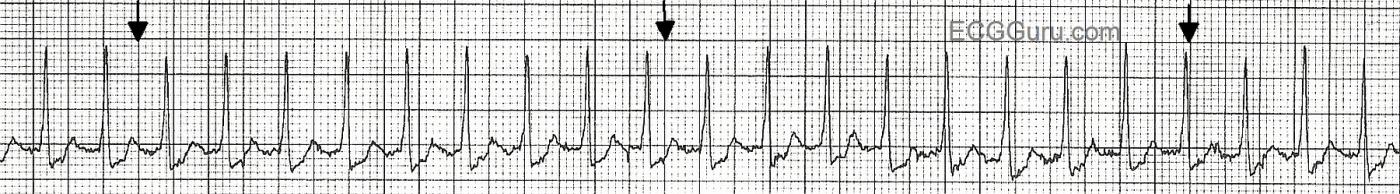
This strip is from a patient who experienced a sudden onset of palpitations and rapid pulse while at rest. It shows a narrow-complex tachycardia, specifically a paroxysmal supraventricular tachycardia. The subject of supraventricular tachycardias is a fascinating one, and is covered extensively throughout this website. The mechanisms of SVT are many, and can be complex for the beginning student to understand. Search the search terms on the left side of the page for entries from ASK the EXPERT and JASON's BLOG for more advanced information about SVT.
For the beginner, it is important to teach the difference between sinus tachycardia and "supraventricular tachycardia". Of course, sinus tachycardia IS supraventricular - but current convention has us using the term "SVT" for atrial or junctional tachycardias, and especially for reentrant tachycardias. Beginner students should understand the function of the sinus node, and it's ability to control the heart rate, based on direction given by the nervous system. The sinus node increases and decreases the rate incrementally, or more gradually than the onset and offset of a reentrant tachycardia. The appearance of a sudden onset of regular tachycardia following a PAC, producing a rhythm with a distinctly faster rate than the original sinus rhythm, is a sure sign of SVT. When the onset or offset are caught on the rhythm strip, our job is SO much easier!
The heart rate helps with the diagnosis. SVTs tend to be faster than sinus tachycardias. SVTs tend to be faster than 150/min, while sinus rhythms TEND to be slower than 150. And patients with sinus tachycardia usually have a readily determined reason for the tachycardia, such as fever, pain, fear, hypovolemia, hypoxia, or exertion. So, a patient on a treadmill for an exercise stress test might very well have a heart rate over 150 / min.
When your students master the understanding of the different behaviors of the sinus node and the reentrant rhythms, and how important patient presentation is to the diagnosis, you will want to add atrial flutter and atrial fibrillation. When these are mastered, be sure to remind your students that atrial flutter can conduct 2:1, and will mimic sinus tach. A good rule of thumb is: Under 150/min.: look for sinus tach first. Around 150 / min.: look for atrial flutter with 2:1 conduction. Over 150/min.: suspect PSVT.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.