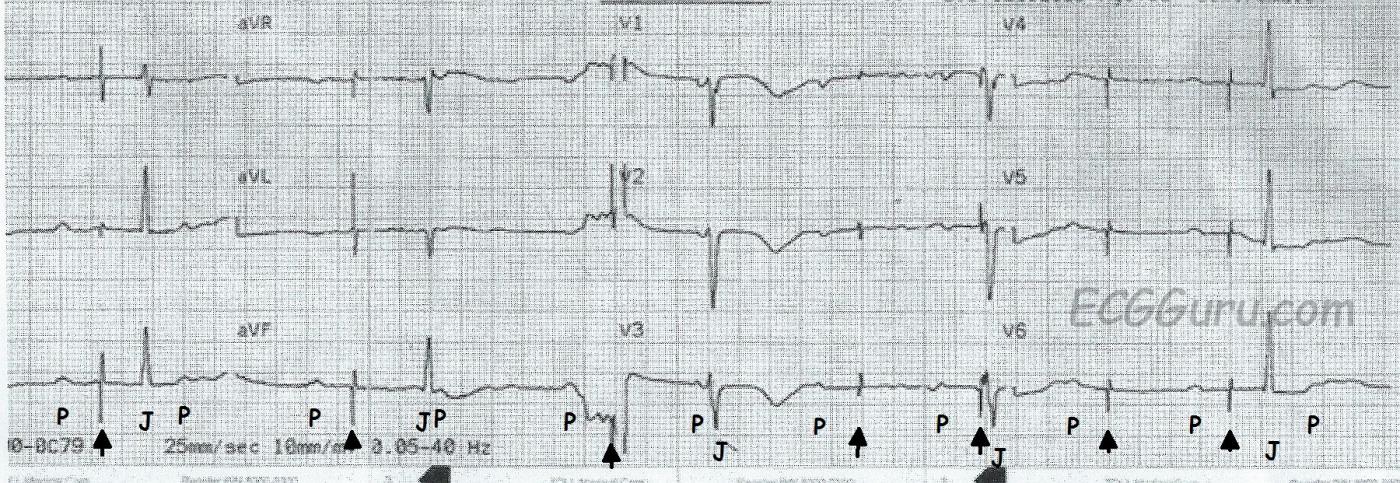
This ECG is taken from a patient with an implanted pacemaker who was experiencing near-syncope. She was taken to the hospital by EMS, where the pacemaker was adjusted to obtain ventricular capture. This ECG did not have a Lead II rhythm strip, so the 12-lead ECG is being presented. The P waves have been marked with a "P", pacemaker spikes marked with an arrow, and the QRS complexes marked with a "J" because they are junctional. Because we can see 12 leads, or viewpoints, the morphology of the P waves and QRS complexes changes each time the machine switches to a new lead.
The underlying rhythm is sinus, with nearly regular P waves occuring at a rate of about 72 beats per minute. The QRS complexes are also regular, but they are dissociated from the P waves. Because the rate is near or just under 40 bpm, and the QRS complexes are narrow, this represents a slow junctional rhythm. Because both atrial and ventricular rhythms are regular, but not associated with each other, an interpretation of complete heart block (third-degree AV block) can be made. This explains why the patient had a pacemaker implanted.
The pacer spikes, for the most part, track the P waves, which is how this pacemaker is programmed. They are not followed by a paced QRS complex, however. This is failure to capture. The second and fourth P waves did not stimulate a pacer spike because of their proximity to the T wave of the junctional beat. The mA (energy setting) was adjusted in the Emergency Dept., and the pacemaker did not require repositioning. The patient regained a reliable paced rhythm.
This section of the ECG Guru is meant to be for your basic students. Pacemakers now have become very complex, with many options and variable settings. So complex, that I would not feel comfortable getting into any more detail than I have here (although visitors to the site are welcome to). It is important that, if you deal with patients in an emergency setting, you do not tell the patient that "something is wrong with their pacemaker" until it has been evaluated by a qualified person who can electronically interrogate the device. It can be very difficult to determine from an ECG how a pacemaker is programmed, and how it should be reacting. Since this patient had symptoms related to the bradycardia, and since pacemaker spikes occurred free of any refractory period and did not produce QRS complexes, it is safe to say there needs to be an adjustment.
In an emergency, with serious symptoms present, a transcutaneous or transvenous temporary pacemaker can be used. Medications such as Atropine, epinephrine, and norepinephrine are also used, depending upon the type of AV block and the resources available.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
What is Wrong? (with the Pacer and with the Patient?)
Interesting tracing - that is presented as a “Basic” ECG - but which also has elements that are not “so basic”.
Ken Grauer, MD www.kg-ekgpress.com [email protected]