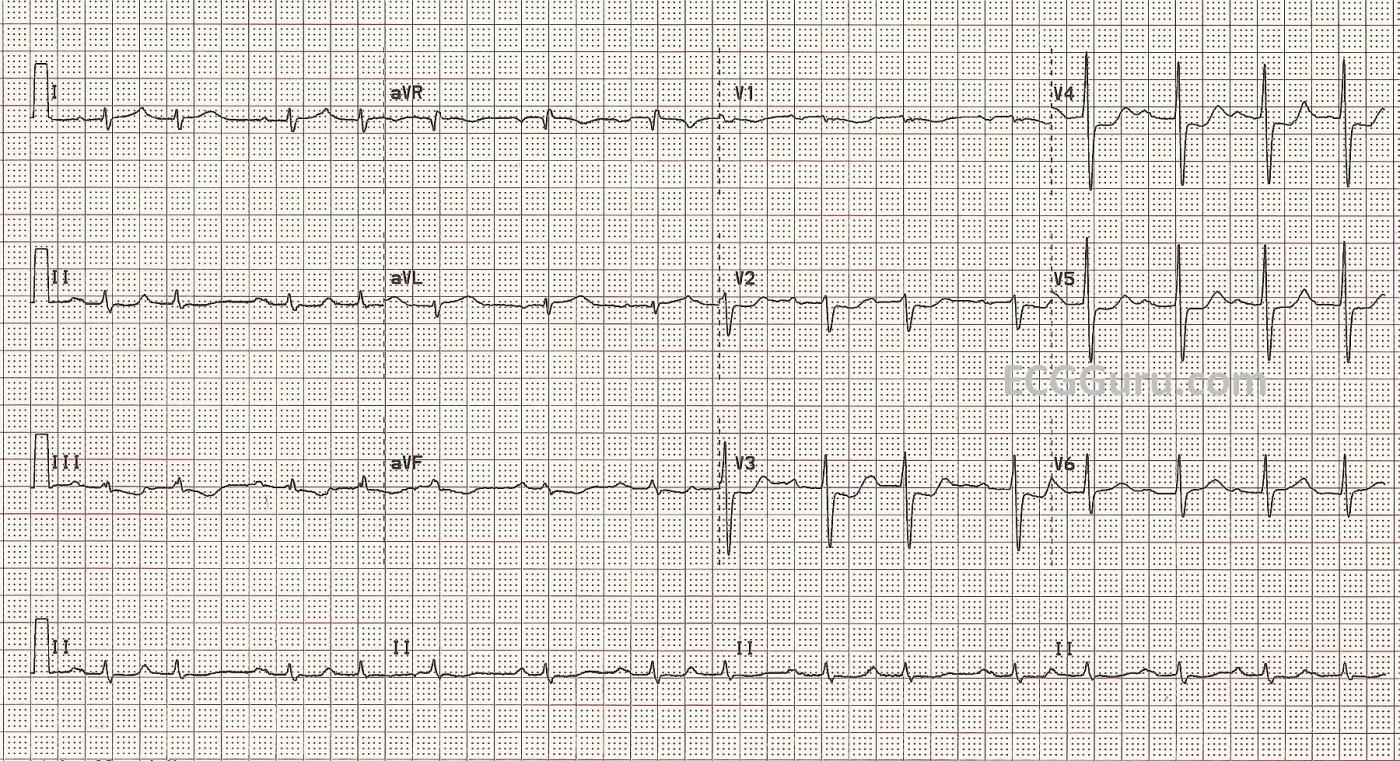
This ECG illustrates what some would call a non-ST-elevation M.I., but may also illustrate the limitations of a standard 12-Lead ECG. This female patient in her 60's presented to the Emergency Department with vague chest discomfort. She was cool and diaphoretic. She gave a history of having coronary artery stents placed in the past. On angiography in the cath lab, she was found to have two stents in her obtuse marginal artery which were occluded. Her case was lost to followup.
The ECG shows ST depression in anterior leads V2 through V6, as well as in the inferior leads, although very subtle. The inferior leads' ST segments are more horizontal than depressed, but flat and horizontal is not normal. She shows a bit of upward concavity or slight elevation in V1, Lead I, and aVL. These signs might be missed by someone looking only for ST ELEVATION. Additional left lateral and posterior leads were not done, and we have to wonder if she would have had some ST elevation in V7 or V8.
Her rhythm is very interesting too. Often, ischemic hearts produce abnormal rhythms, and it is not unexpected. The rate and the rhythm caused this patient no difficulties during her time in the ED. On first glance, her QRS complexes appear to be "grouped", as they would in a Wenckebach type block. On closer inspection, you will see two distinctly different P waves, and no non-conducted P waves. This appears to be a sinus rhythm with frequent PACs. The PRI is prolonged at .28 sec., which also is not unusual for M.I. patients.
We are very interested to hear what YOU think about this interesting ECG, including the rhythm. We are hoping to hear from people from all areas of cardiac care - what do you think are the main teaching points of this case?
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
ECG of week July 28th,2013
This 12 lead looks very much like a posterior MI with ST inversions in leads V2,V3, & V4. If you invert the ECG and look "through" the ECG you will find the ST segment elevated as if you're looking at the heart from the posterior side.This 'trick of the trade" was shown to me by a cardiologist. It is a great ECG.
Dave Kemper
I agree...
Dave, this ECG was given to me by a colleague, and I wasn't present when this patient was in the E.D. I have always wished I had a V7 and V8 to look at the lateral / posterior wall better. But, then, a definitive diagnosis was made very quickly in the cath lab. Luckily for this woman, she was brought to a full-service cardiac hospital. It is good for all of us to remember that acute M.I.s don't always present with ST elevation.
Dawn Altman, Admin
PR
Do I see group beating? Type 1?
I see two different P waves
Hi, Marionnurse:
I see P waves with two distinctly different morphologies. Of course, it would be great to have a much longer rhythm strip. I proposed a sinus rhythm with PACs. Type I block should have non-conducted P waves. I hope other ECG experts will weigh in.
Dawn Altman, Admin
Very interesting case!
This is a great case, thank you for posting!
I am not really sure about my findings this time, I´m looking forward to the corrections from the gurus :)
The RHYTHM is irregular, there is a hint of grouping in some parts of the ECG. I tried to find a pattern with my calipers and made a laddergram. It was very hard, because there are several morphologies of P waves (at least 3, propably 4) and even more "types" - of PR intervals.
One of these types (in three P-QRS) had constant PR interval, upright P waves in II, III, aVF, aVL and inverted P wave in aVR. I considered these P waves SINUS. The rest of the P waves were different and/or had different PR interval - they looked like PACs to me, BUT it´s hard to say what is PREMATURE in here, because I didn´t find two consecutive sinus P waves in a row.
This is my laddergram: https://www.dropbox.com/s/qxeo8asng9gu20p/CAD107.jpg
It is the best I was able to come up with. I know that it is propably incorrect, I may have been putting too much weight on different PR intervals! Or the changing PR could be due to AV nodal impairment. Please correct me! IF the laddergram is correct, I think this could be described as Multifocal Atrial Rhythm (MAR) or sinus rhythm with multiple PACs - As dr. Grauer says - they are on the same spectrum. If we treat the underlying problem (with PCI), the rhythm probaply diseapears..
The rest of the ECG:
Impression:
Sinus rhythm with multiple PACs OR Multifocal Atrial Rhythm. Posterior STEMI, possible lateral wall involvement.
Thank you for this case!
- See more at: http://ecgguru.com/comment/reply/477#sthash.mAqeaygH.dpuf
The "THEME" of the ECG Counts Most ...
I am writing this Comment "on the road" (= reduced to ipad without calipers) - so a bit more challenging to comment on. VERY interesting tracing - with already great participation from others! I think this tracing is one where one needs to STEP BACK and look at "the Forest" rather than the trees ...
The history is telling. The patient has a history of CAD (prior stents) - and she is obviously ill ("cool & diaphoretic" ) - albeit without clear timeline of her symptoms. This doesn't necessarily sound like a "new-onset crushing chest pain" - so I sense a background of significant CAD with recent exacerbation. To me - this is consistent with her tracing.
The rhythm is problematic. I am admittedly having trouble telling what is sinus and what is atrial ectopic from how many different foci ... That said - it is "the THEME" that counts. There is underlying sinus rhythm, albeit with 1st degree AV block (which of itself could be significant given potential acuity of her CAD presentation). I interpreted this as multiple PACs. Despite group beating - it is not AV Wenckebach, because the atrial rate isn't constant and there is no consistent progressive PR prolongation. Instead - I think the "group beating" is due to certain PACs that repeat with fixed coupling. Use simultaneously recorded leads (look at 4 leads at once to confirm that PACs are happening! - which I do from P wave appearance in several simultaneous leads). This isn't MAT - because some pattern IS present with regularity of those repetitive PACs.
I actually looked VERY carefully for the possibility of MAT - because there are features on this tracing consistent with longstanding pulmonary disease (low voltage in the limb leads; S wave in lead I without QRS widening; persistent precordial S waves) - but MAT is not present.
The most striking finding on this tracing is diffuseness of the ST flattening-depression. This is seen to varying degrees in the 3 inferior leads plus leads V1-thru-V5. Especially in view of subtle-but-real ST elevation in lead aVR -I think this pattern strongly suggests a background of probable 3-vessel (at least) CAD that appears to be longstanding. We need to remember that hers is not a "virgin circulation" - as she has already had stents - so localizing predictions may not be optimally accurate (she has had stents; she probably has collaterals).
In addition to that subtle ST elevation in aVR - I think there is also subtle-but-real ST elevation in lead aVL. ST elevation in lead aVL but not in anterior precordial leads IS consistent with acute circumflex obtuse marginal occlusion - though I don't know that I would have called this based on this tracing.
As to possible acute posterior infarction - leads V2,V3,V4 in isolation are certinly consistent with this. We see a relatively larger-than-expected increase in R wave between V2-to-V3 with that peculiar shape of ST depression in these leads that yields a highly suggestive positive "mirror test". That said - I think the "THEME" is more important in assessment of this patient's 12-lead. To me that "theme" is of diffuse ST depression except for subtle ST elevation in aVR and aVL - which strongly suggests significant severe CAD rather than localization to the posterior wall. Given age of the patient, her prior documented history of CAD - and obvious profound symptoms ("cool and diaphoretic" but without clear new-onset chest pain) - I sense a NON-acute-STEMI picture - but one that nevertheless merits stat consultation with cardiology for immediate cath with expectation that acute angioplasty of one or more lesions will be forthcoming. GREAT case for discussion.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
A Really Interesting ECG!
Dawn...
It has obviously taken me 3 years (!) to see this presentation and I'm really glad I found it.
First, regardless of her past medical history, this is a patient who is acutely ill - one does not become cool and diaphoretic for nothing!
Second, I want to invoke my own Jones's Rule: ST depression in a patient with chest discomfort who is cool and diaphoretic (i.e., with symptoms compatible with an ACS) represents reciprocal change until proved otherwise. We see obvious ST depression in the inferior leads with some arguable (i.e., difficult to be absolutely sure) ST elevation in aVL. I don't have to see ST elevation in aVL to satisfy myself that this patient is most likely having acute lateral epicardial ischemia. The lack of ST elevation in aVL is not surprising nor is it unusual. STE in Lead aVL often follows the reciprocal changes in the inferior leads. I also think the ST depression in V2 through V4 and probably even V5 represents an extensive acute posterolateral epicardial MI. I considered Lead V1 almost uninterpretable until I viewed it upside down and backwards. When viewed from that perspective, its changes become a bit more perceptible. This maneuver has been around for many, many years (I was first taught it in 1970!).
I do agree with Dr. Grauer that there is most likely more extensive, diffuse circulatory compromise. The LAD and the ramus intermedius (if present) should be supplying circulation to the area covered by V5 and V6 but that does not appear to be the case here, which tells me that there is also probably some disease in the LAD as well. I'm sure the STE in aVR is alerting us to the presence of at least some subendocardial ischemia, though I would expect the ischemia to be worse in the lateral precordial leads if this was primarily due to subendocardial ischemia/infarction.
But my main interest is in the unusual rhythm that is seen so clearly in the Lead II rhythm strip. First of all, remember that this is a proven occlusion of the left circumflex (LCx). Although the LCx is dominant only 10 - 15% of the time, it provides the artery to the sinus node 40% of the time no matter which artery is dominant. And the artery to the sinus node is the main supplier of circulation to the right atrium. OK...
We definitely have two - and likely three - different P wave morphologies in the Lead II strip. The 1st and 3rd P waves constitute one morphology, the 2nd and 4th P waves another morphology and I think the 5th QRS is preceded by a shallow, inverted P wave. To get a good measurement of the normal PR interval, measure the 1st or 3rd PR interval in the V3 strip. Getting back to the Lead II rhythm strip, I think the 1st and 3rd P waves represent sinus P waves. The long pause after the 2nd P wave shows us that the T wave in Lead II is isoelectric and in Lead III we can see a separation between the inverted T wave and the P wave that follows. So in the Lead II strip, those are all P waves (or P' waves) and not T waves: no P wave is hiding in a T wave in Lead II (at least not until the very end). If you map out the sinus P waves in the Lead II rhythm strip, they do OK except in the vicinity of the 5th QRS complex with the premature, inverted P' wave. However, if you keep mapping it, it does OK for a few beats and then things fall apart toward the end of the strip when the P waves no longer map out (because the sinus rate increases significantly).
Now, let's do the same beginning with the 2nd P' wave (let's assume the distance between the 2nd and 4th P' waves is our P'-P' interval). Set your calipers to that interval and begin mapping out the P' waves. We have a bit of a hiccup around the 5th QRS just as before, but if we keep mapping out the P' waves everything falls exactly into place all the way to the end. Also, if you compare the P-P' intervals in the Lead II rhythm strip (the coupling intervals), they are not always the same.
Here's what I strongly suspect: there is an atrial parasystole here and the first parasytolic interval that we can see is from the 2nd to the 4th P wave (the P' waves). It appears to fail us around the 5th QRS complex (the 3rd P' wave is late). But if we keep mapping the P' waves, they appear to continue as though nothing happened. I think the 5th P wave (premature, inverted) depolarized the area around the atrial parasystolic focus and caused a first degree exit block. It also managed to reset the sinus node which probably fired shortly afterwards into atrial tissue that was still too refractory to conduct - but it did manage to prolong the refractoriness. The parasystolic impulse was able to eventually exit, but not without some delay. However, the inverted PAC was not able to enter the parasystolic focus and reset it. That's why it appeared to pick up right where it left off. But most notably, toward the end of the Lead II rhythm strip, the sinus rate appears to increase significantly, but the parasystolic rate does not. I think this is the best argument for a parasystolic atrial focus. If the P' waves were coupled to the sinus P waves in a re-entrant manner, their rate would have initially increased in parallel with the sinus rate.
So, in essence, the 1st P wave is a sinus P wave, the 2nd P wave is parasytolic and the 5th P wave (shallow, inverted) is simply an ectopic PAC from the low atrium (it is too far in front of the QRS to be junctional).
Thanks for a great website, Dawn.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Another look at what may be happening here...
I debated whether to bring this up in my initial post (it is a bit complicated) and then I thought "Heck... why not?"
A Japanese cardiologist named Dr. Kinoshita (I'm not sure if he is still practicing or even if he is still among us) introduced (or rather expanded on) a very novel concept of parasystole. It has not really made its way into the introductory-to-intermediate-level literature and actually very few advanced electrocardiographers are familiar with it. It is a complicated concept and, unfortunately, it takes all the "magic" out of parasystole. Parasystolic imperviousness to interference by sinus impulses has created a parasystolic lore somewhat akin to Harry Potter's "cloak of invisibility." Kinoshita showed that the entrance block was less "magic" and more an issue of impulse timing and refractory periods.
A parasystolic focus is a cell or cells that have the attribute of spontaneous phase 4 depolarization. Normal working cells do not have this ability unless they become so diseased that the sodium channels are no longer functional while the If ("funny") current and the calcium channels are still functioning. However, cells within the Purkinje system and the atrial conducting pathways have this ability normally. Therefore, it makes sense that any parasystolic focus is either going to be in one of these pathways or in a "side" or branching pathway. There appears to be a "front door" and a "back door" to these parasystolic foci, which only makes sense: if they are in a conducting pathway, then that focus can be approached via antegrade and/or retrograde conduction.
The following explanation is a bit of an over-simplification, but here goes...
The antegrade ("front door") approach is typically an all-or-nothing phenomenon. Either the approach is closed due to refractoriness and the parasystolic focus is protected or it is not, and the antegrade sinus impulse enters the parasystolic focus discharging and resetting it. The retrograde ("back door") approach is prone to Wenckebach (i.e., delayed) conduction. The retrograde impulse, after some delay, manages to enter the area of the parasystolic focus. If it finds the focus non-refractory, it can discharge and reset it; but if it finds the focus refractory, it has no effect on it. However, it can exit the area of the parasystolic focus (out through the "front door") and re-excite the myocarium as a reentrant premature ectopic complex (PAC in the atria, PVC in the ventricles).
That could very well be what has happened in this tracing. The late "parasystolic" P' (5th P wave) is probably not actually a parasystolic beat itself but rather a reentrant PAC. While the retrograde impulse from the sinus node was able to traverse the area of the parasystolic focus, it neither discharged nor reset the parasystolic pacemaker itself. That is why the atrial parasystole was able to resume its rhythm right on time.
Alas, there is no protection of the parasystolic pacemaker by a "magical" entrance block. In the end, it all boils down to timing of impulses and refractoriness of the surrounding tissues.
Dr. Kinoshita's writings on this topic extend back many, many years and are generally available online. The complexity of the topics he chose to write about require (sometimes) weeks of study. Although he lived and worked in Japan, it is not a language issue that makes the papers complex reading - the English is very clear and impeccably correct. He simply chose to tackle the really difficult questions.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Thanks so much.
The explanation you give makes sense to me, and if Dr Kinoshita's writings are challenging for you, I think I will stick with your version!
Maybe one day when I have a very clear mind, I will take a look. One thing I really love about medicine and ECG is that you NEVER get to the end of learning you can never know it all.
Dawn Altman, Admin