Submitted by jer5150 on Sat, 03/09/2013 - 10:31
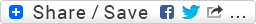
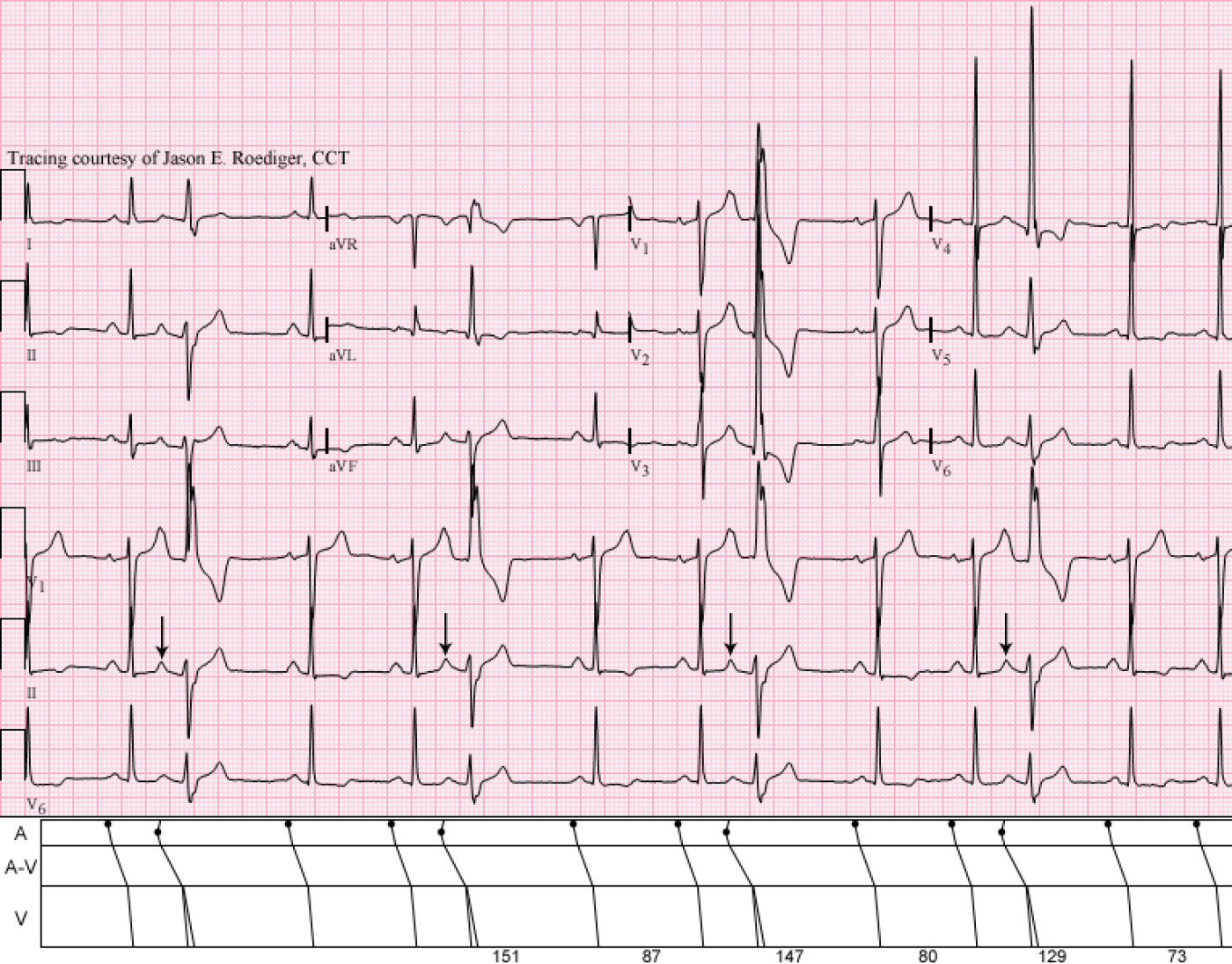
These are two 12-lead ECGs that I performed on two completely different patients several years apart.
Patient's clinical data (Top ECG):
57-year-old black man
Patient's clinical data (Bottom ECG):
67-year-old black man
Are both of these ECGs showing the same rhythmic pattern?
Rate this content:
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Nice CASE!
Hi nice tracings!
I think that these two are different.
The first one is showing atrial trigeminy (with RBBB aberation), while the second one is showing ventricular trigeminy.
Here is what lead me to this conclusion:
- Tracing A: has hidden P waves in the preceding T waves and the ectopic beats have RBBB morphology (in all important leads - V1, I, V6. Plus incomplete compensatory pause.
- Tracing B: I don´t see hidden P waves. The compensatory pause is complete. It resembles RBBB too, but not so much. And the QRS in aVR seems too wild.
I´m looking forward to the right answer. Thank you very much for posting such interesting case!
The P Waves Provide THE Clue!
Jenda (I assume Jan = Jenda?) - I believe that Jason intentionally chose these 2 tracings for you (based on your questions about compensatory pauses yesterday)!
I agree with your astute interpretations Jan! Atrial trigeminy for the TOP Tracing - with RBBB/LAHB aberration of each PAC. As you indicate - the T wave preceding each wide beat is peaked (best seen in the lead II rhythm strip) - confirming that these are PACs. The QRS pattern in lead V1 looks a bit atypical for RBBB (hard to tell what the QRS really looks like in this lead given all the overlap ...) - but typical wide terminal S waves are seen in leads I,V6 - and the predominantly negative QRS (rS) pattern in lead II is consistent with LAHB aberration.
The LOWER Tracing is a bit tricky! I say this because the T wave preceding each wide beat is different, albeit not really with a peak or notch suggesting a premature P wave. This IS confusing ... - BUT as you state Jan - there is a perfectly compensatory pause. Much MORE important than the pause containing the PVC being precisely twice the sinus R-R interval is the fact that you can MARCH OUT THE P WAVES (best seen in lead II of the Lower Tracing) by the notch that occurs right on time in between the end of the PVC and the beginning of the ST segment. This (much more than just being "compensatory" ) proves that these must be PVCs. I have no idea why the ST segment of the beat just before each PVC looks a bit different - sometimes patients with ischemia may manifest this phenomenon, but impossible to tell without a longer tracing and more normal beats to assess what the ST segment of sinus beats truly looks like.
VERY interesting! THANKS for posting - : )
P.S. PVC morphology in the Lower Tracing is left ventricular - probably with site of origin close to the left posterior hemifascicle.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
I see the trigeminy in both
I see the trigeminy in both ECG. My questions are: Is there such a thing as "Junctional Trigeminy"? If so, could you consider the 1st to be a Junctional Trigeminy since the QRS is wider than the regular beats even though there are upright P-waves present? Or is this coming from the bottom of the atria close to the junction?
Trigeminy
@authorannegriffith - Yes, there is such a thing as "Junctional Trigeminy" however those are not junctional premature beats (JPBs) occurring every third beat in the 1st ECG. There are multiple forms of ectopy in trigeminal patterns but ventricular and atrial are by far the most common. Comparatively, JPBs are much more rare and don't usually occur in repeating patterns. More often than not, JPBs conduct with a QRS morphology and width that is identical to those seen on the surrounding sinus beats - unless the JPBs are conducting with aberrant ventricular conduction. In the 1st ECG, the preceding upright P'-waves in lead II would exclude these from being JPBs.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]
Super! Thanks for the
Super! Thanks for the clarification!
INTERPRETATION
Unfortunately, I think Ken was giving me too much credit in deliberately posting these ECGs as I’ve been wanting to feature both of these on the ECG Guru before Jenda made his comment but their posting was fortuitously timely none the less.A common theme/thread here is the repeating pattern (i.e., “trigeminy”) and the taller left peaks (so-called taller left “rabbit-ears”).
This is what Dr. Marriott referred to as a “mutual mimics” or “unheavenly twins”. The concept being that whenever you see what you believe to be VPBs – you should think of and exclude APBs with aberrancy.
One of the reasons why I like this pair of ECGs is because the extrasystoles can be directly viewed in each of the 12 individual leads allowing one to determine QRS morphology and axis.
In the differential diagnosis of VPBs versus aberrant APBs, there are three things to look for: (1.) The presence or absence of preceding P’-waves, (2.) QRS morphology (esp. in leads V1, V6, and I), and (3.) Duration of the postextrasystolic cycle. Here, the QRS morphology in lead V1 is of little help.
INTERPRETATION (Top ECG):
1. Slightly irregular sinus rhythm (rate about /min) interrupted by . . .
2. . . . atrial premature beats (APB) occurring ever third beat producing one form of . . .
3. . . . atrial “trigeminy” and conducted with . . .
4. . . . right bundle-branch block plus left anterior hemiblock (RBBB+LAHB) aberration
COMMENTS:
This patient exhibited no less than 3 different varieties of ventricular aberration (not show here). At other times, APBs were conducted with just RBBB aberrancy and then with RBBB plus left posterior hemiblock (LPHB) aberrancy. This may be hinting towards some latent infra-Hisian disease. At no time did this patient display either normally conducted APBs or nonconducted APBs.
Here, the APBs display a left axis deviation (LAD) whereas the sinus beats all have a normal axis.
The aberrant ventricular conduction is not just taking place in the right bundle-branch (RBB) but it is also taking place in the left anterior fascicle (LAF) as well making the aberrancy “bifascicular”. I should note that as of 2009, the AHA, ACC, and HRS no longer recommend use of the term “bifascicular” anymore. As an alternative, they recommend fully spelling out the specific part of the His-Purkinje system that is involved which is exactly what I’ve done in line 4 of the interpretation above.
Admittedly, these aberrant APBs are not terribly wide in duration measuring at only 0.13s in duration.
I’ll go on record as saying that pure and uncomplicated RBBB will not produce a taller left peak of its own in lead V1. Pure RBBB always produces a taller “delayed peak” due to the sequence of electrical activation in the ventricles. When RBBB is complicated by a true posterior infarction, this represents one other occasion when lead V1 will produce a taller left peak.
If this patient were to have gone into some form of supraventricular tachycardia (SVT), there is a real chance that it could have conducted with the same QRS morphology seen above in the aberrant APBs and possibly lead one to mistakenly make the wrong interpretation of ventricular tachycardia originating from the left ventricle.
Interestingly, the sinus node recovery time (SNRT) is reciprocally shortening in directly correlation to the progressively increasing sinus rate.
INTERPRETATION (Bottom ECG):
1. Sinus rhythm (rate = /min) interrupted by . . .
2. . . . ventricular premature beats (VPBs) presumably originating from the left ventricle (LV) and occurring every third beat producing one form of . . .
3. . . . ventricular “trigeminy”.
4. Possible left atrial enlargement (LAE)
COMMENTS:
QRS duration is “wide-wide” at about 0.15s.
The VPBs have a frontal plane axis in the upper right quadrant. This axis alone would heavily favor an ectopic ventricular origin. Initial left peak taller than the right (seen in about 55% of all ectopic beats originating from the LV). Similarly, left VPBs are associated with an rS complex in lead V6 about 55% of the time.
In summary: the sole value of the “rabbit-ears” clue is that when the left peak is taller than the right, the odds (about 10:1) are heavily in favor and evidence of LV ectopy (i.e., > 90% likelihood).
In lead aVL, the VPBs look deceptively similar to the conducted sinus beats.
If this patient were to develop ventricular tachycardia with an identical QRS morphology and axis, then there are enough clues present in order to be certain of the tachycardia’s origin.
Compare the axis and morphology, of the VPBS in each lead of my ECG, to the left ventricular tachycardia on this 12-lead ECG:
http://europace.oxfordjournals.org/content/early/2007/07/12/europace.eum129/F1.large.jpg
Reference:
1. http://hqmeded-ecg.blogspot.com/2013/05/pvc-or-aberrant-conduction-another.html
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]