Patient’s clinical data: Symptomatic 49-year-old white man who presented to the emergency department (ED) with left-sided chest pain.
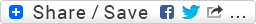
At the time of admission, there were two consecutive 12-lead ECGs initially performed in the ED. The above ECG was the second of the two that was performed. Why would there be a mandatory need to perform a minimum of two ECGs on this type of a patient?
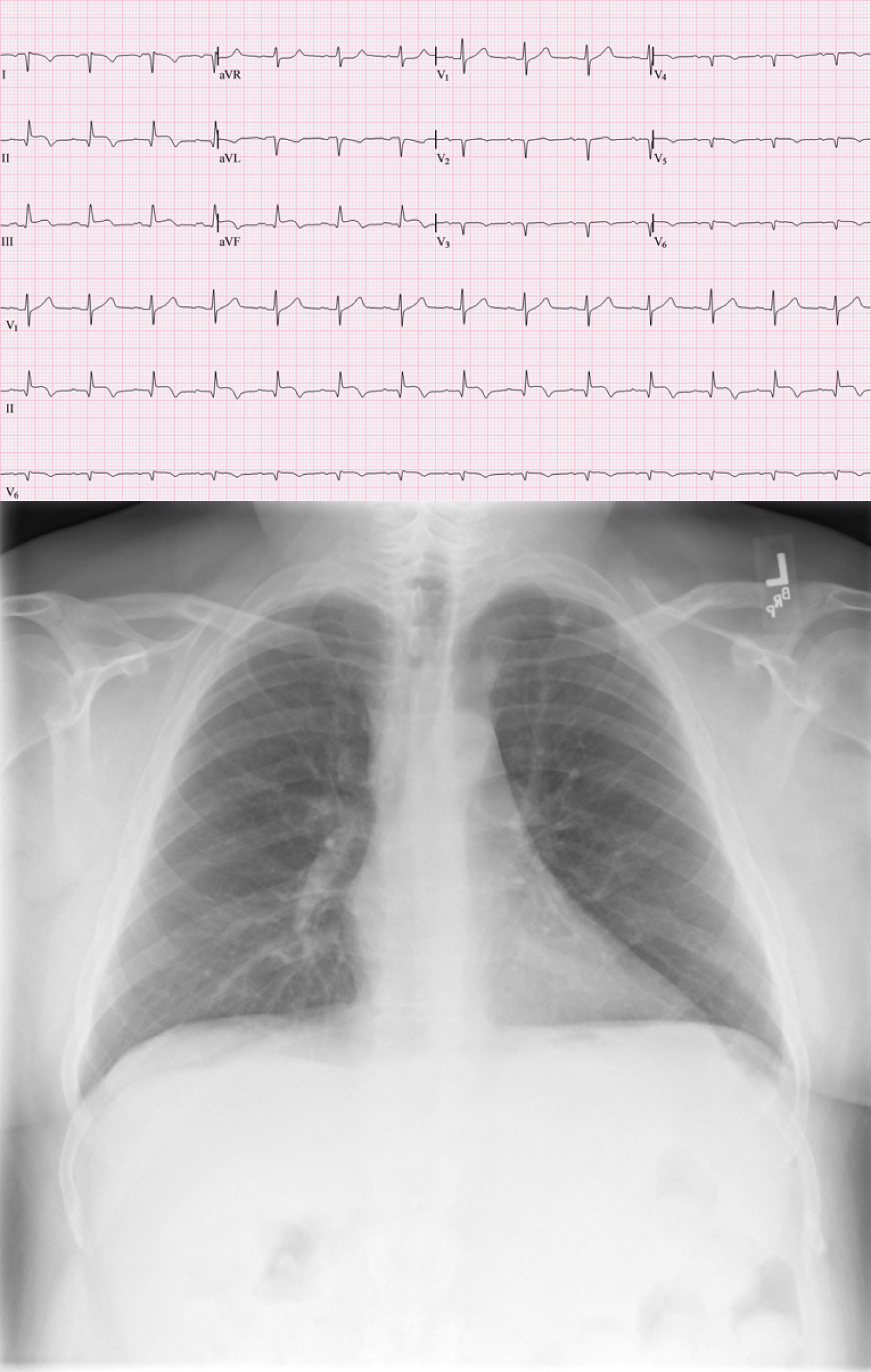
** *** Both of these images are from the same patient. Please note that the patient’s chest film was performed correctly and is anatomically accurate (i.e., situs solitus) *** **
I’ve included the chest X-Ray (CXR) because it, by far, provides more clarity than an ECG alone ever could.
Questions:
(1.) What emergent event has brought this patient to the emergency department?
(2.) What has produced this unusual combination of QRS axis and precordial pattern?
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Hi
Infer-MI and maybe lead reversal?
Greetings marionurse!
The answer to your question is: Yes and Yes. The CXR proves that there is indeed a lead reversal.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]
INTERPRETATION
The 12-lead ECG was performed in the emergency department on a patient having an acute inferior infarction. Initially, the technician performed a "standard" ECG. Upon completion of the first ECG, the tech was either instructed by an ED physician to perform a second ECG to obtain a right-sided series or they had a standing protocol to do so in the event a patient presented with this specific type of infarction. WHAT THEY DID RIGHT: The tech correctly placed the precordial electrodes and attached the cables so that they are now monitoring leads V1R through V6R (a full rather than a partial right-sided series). This was done in an attempt to determine if there is any right ventricular (RV) involvement (esp. in leads V3R and V4R). WHAT THEY DID WRONG: The tech needlessly switched the right arm and left arm cables so that the overall ECG now superficially mimics a patient with mirror-image dextrocardia having an acute inferior infarction while having their ECG configured in a convention "standard" placement. In the ECG, lead II is really lead III and lead III is really lead II. Leads aVR and aVL are also transposed. Lead I is, or course, inverted. The tech probably knew that there are two primary occasions when you perform a right-sided series and they got confused. There was no reason for them to reverse the RA and LA cables.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]