Submitted by Dr A Röschl on Fri, 07/26/2024 - 02:19
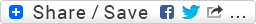
This is the ECG of a 50-year-old man with a congenital heart defect (we do not have exact details).
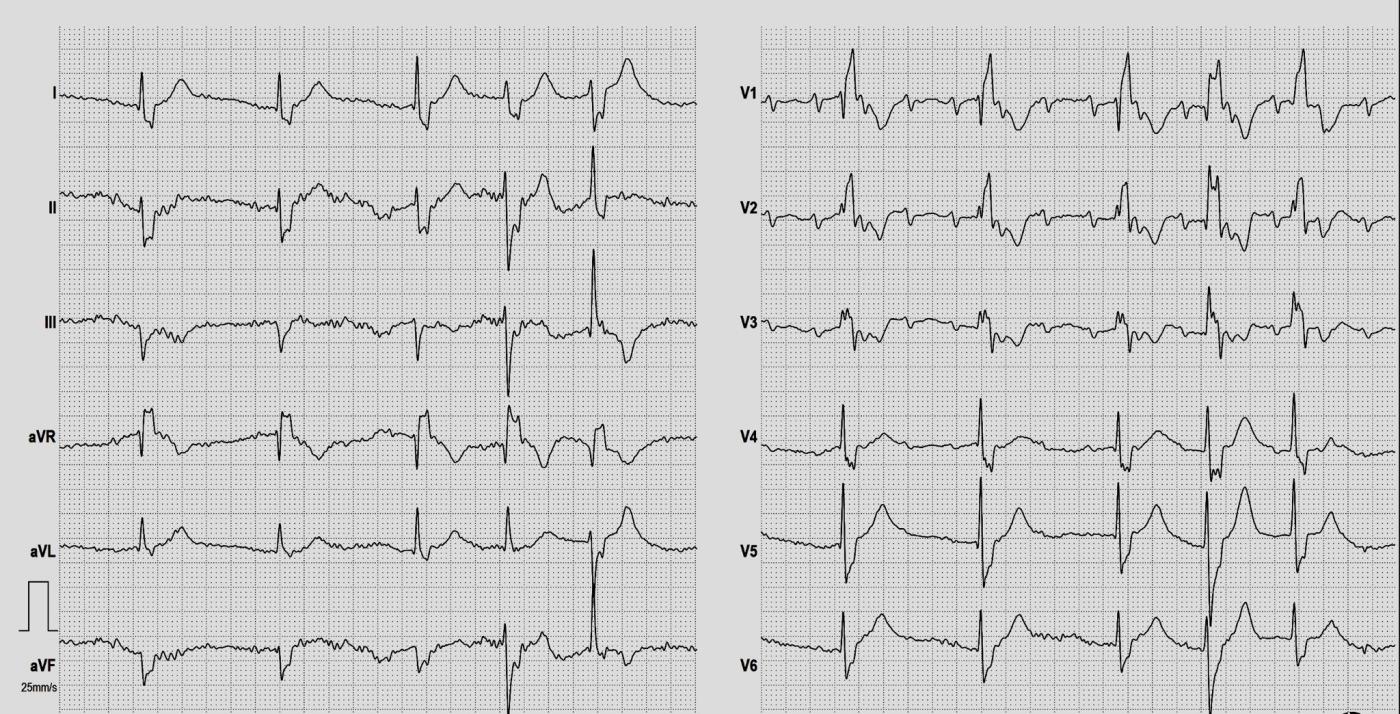
To interpret an ECG with several different abnormalities, you have to proceed systematically. You can see my comments in the second picture. Perhaps Dawn would like to add something?
Rate this content:
-
- Dr A Röschl's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Interesting ECG with multiple abnormalities
Thank you, Dr. Roeschl, for this interesting ECG. I agree about being methodical, so here is my take on it.
The limb leads and the chest leads appear to be run simultaneously over about five seconds (the regular and irregular beats match up). So I used the chest leads for interpretation of the rhythm, as the P waves were much clearer. Muscle tension artifact and small P waves handicapped the limb leads.
The underlying rhythm (P waves) appears to be a supraventricular tachycardia (could be ST) at about 161 bpm (measured with computer screen calipers). There is 3:1 conduction, resulting in a ventricular rate of 54 bpm. The PR interval is 234 ms. With a tachycardia, periodic non-conduction of the AV node could be normal if all the non-conducted P waves land on the preceding T waves, in the refractory period. ("Physiologic Block") If P waves are "out in the open" and still fail to conduct, we have to consider AV block. In the setting of chronic tachycardia, this may be due to medication given with the intention of slowing the heart rate. Clinical correlation is essential here.
At the end of the strip, there are two beats that look different. I agree that they are probably PVCs that have merged with the supraventricular impulses (fusion beats). The first one starts right on time with a normal PRI for this strip, so I believe the normal conduction is represented first, with the ventricular conduction coming from below altering the shape of the QRS a bit. The second one (last ventricular beat on the strip) starts a bit early with a shorter PRI - which isn't a PRI at all, as the PVC starts before the supraventricular beat reaches the ventricles. In some leads, this beat looks very much like the first, conducted, three beats on the strip, but in others, it looks quite different. So, I would call this a PVC, but I would not correct anyone who calls it a fusion beat. The clinical significance is zero.
As for the more "normal" beats - they are not normal at all. As Dr Roeschl pointed out, they are wide, and are conducted with a right bundle branch block pattern. In addition, the frontal plane axis is leftward, indicating a left anterior fascicular block. This is a common conduction block combination, as the RBB and the LAF have a common blood supply.
Clinically, I would concern myself with: why is there an underlying SVT? And also, what gave us the 3:1 block? Most likely, this was done intentionally with medication, because who wants a heart rate of 161?
To continue being methodical, I woud look at the ST segments and T waves. In RBBB, I expect normal T waves to be directed opposite the terminal part of the QRS. So, all those "inverted T waves" are fine. I don't see ST elevation or very abnormally-shaped ST segments, although the bases of the T waves in I and aVL, as well as in V5 and V6 are wide. A repeat ECG would help us decide if this is an acute or evolving change.
In all ECGs, clinical correlation is very important. Are these abnormalities new or chronic? Are they affected by medications that have been given? Are they consistent with any symptoms? How old is the patient? (In the above case, we know he is a 50 year old man). What is the past medical history, and what co-morbidities exist? (In the example here, we know there is some type of congenital heart defect).
Thanks again for the workout, Dr. Roeschl.
Dawn Altman, Admin
I'll Play "Devil's Advocate" — I vote for Aberrant Conduction
My attention was drawn to this interesting ECG providing by Dr. Roeschl. Rather than 2 PVCs at the end of this tracing — I will play "Devil's Advocate" by saying I believe both of these final beats are aberrantly conducted supraventricular impulses.
First, to emphasize 2 points by Dawn = #1) The same 5 beats are shown in both the limb leads and the chest leads. So our conclusions are based on a total of only 5 beats — of which 2 of these 5 beats look different primarily in the limb leads; and #2) Whether I am correct — or Dr. Roeschl and Dawn are correct — does NOT have any influence on clinical management, because the atrial tachycardia is the primary disorder. BUT — I find this an interesting discussion point that is instructional in illustrating that more than a single answer may be contemplated.
Looking first at the chest leads — ALL 5 beats seemingly show RBBB conduction in lead V1 (albeit with slight variation in QRS morphology in this artifact-laden tracing in which there is marked fragmentation of the QRS complex). But note the IDENTICAL (and NARROW) initial deflection of ALL 5 beats in leads V4,V5,V6. This is NOT what I would expect if beats #4 and 5 were PVCs. And note that each of these 5 beats in the chest leads have a wide, terminal S wave — as would be expected with RBBB conduction (ie, Seeing the appearance of these 5 beats in the chest leads suggests all 5 beats are supraventricular with RBBB conduction).
Now look at the limb leads. Although the 5th beat (that is labeled in green as a "PVC/PVC-fusion beat") looks different — it also has a VERY narrow initial deflection AND a QRS morphology in leads I, II, III that is typical for LPHB conduction. It is NOT uncommon for changes in R-R intervals in a complex arrhythmia to alternate between LAHB and LPHB conduction.
The 4th beat (that is labeled in blue as a "PVC") also looks different from the first 3 beats — but it too begins with a VERY narrow initial deflection —and it manifests a QRS morphology INTERMEDIATE between the RBBB/LAHB morphology of the first 3 beats and the RBBB/LPHB morphology of the 5th beat. I favor postulating in this patient with obvious severe underlying heart disease who manifests impaired conduction over the right bundle branch AND both hemifascicles in the left bundle branch — that this patient manifests an "intermediate" conduction pattern for beat #4 in transition from switching from RBBB/LAHB to RBBB/LPHB.
GREAT case for discussion — and our THANKS to Dr. Roeschl — :)
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Good Reminder
Thank you, Dr. Grauer, for your insight. It is a great reminder to look at the initial deflections in wide-complex beats.
Dawn Altman, Admin
Agreed!
Hi Ken, thank you very much for your comment. I have looked at the ECG again and I think you are right with your comments (as is practically always the case). I will try to find more ECGs from this case to be even more sure. Having Ken Grauer as a backup for tricky ECGs is always great! Thanks again!
We ALL Learn from Each Other Every Day
Hi Andreas. Your work is OUTSTANDING! The purpose of the ECG Guru is to foster interactive discussion from which we ALL learn. Would be great if you were able to find additional ECGs on this patient. Distinction between ventricular beats vs aberrant conduction in an irregular supraventricular rhythm can be exceedingly challenging. Finding a longer period of ECG monitoring on this patient would probably add certainty as to which beats are ventricular vs aberrantly conducted. KEEP UP those great cases you are posting on ECG Guru! — :) Ken
Ken Grauer, MD www.kg-ekgpress.com [email protected]