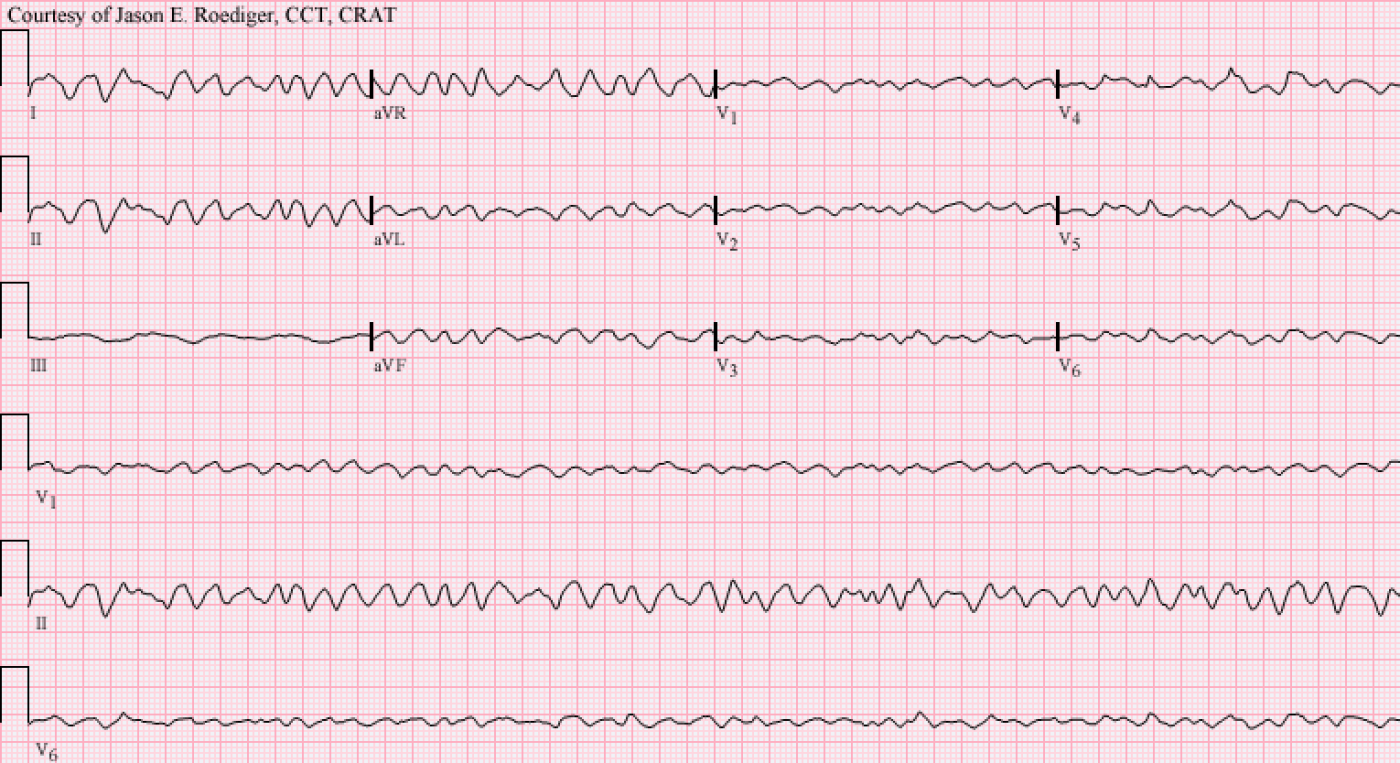
Chances are that just the mere sight of the 12-lead ECG above has already piqued your interest in what will follow! It was recorded during an actual code-blue and the patient expired a short time later but I'm posting it here in order to graphically illustrate my point. Incidentally, the above ECG was diagnosed by my former Chief of Cardiology as "Wide QRS Tachycardia" but is clearly "amorphous" ventricular fibrillation.
HYPOTHETICAL SCENARIO:
You are working an unremarkable evening shift on a cardiac step-down ward when your patient on telemetry abruptly converts from normal sinus rhythm at a rate of 70/min into ventricular fibrillation (V-fib). Immediately, a cacophony of bells and whistles are urgently alarming all around you. You and the rest of the "cavalry", with crash-cart in tow, spring into action and burst into the patient's semi-private room only to find them calmly relaxing in bed and quietly watching television. What the *!#/%&??? Not at all what you were expecting to encounter. You were anticipating a need for deploying the defib pads, artificial ventilations, chest compressions, and copious amounts of epi. The patient and their roomate both look horrified at the complete lack of the social graces exhibited by the staff at this late hour. You glance at their bedside monitor and it is still displaying V-fib. The patient is completely oblivious to your concerns and has not a care in the world as they continue to flip through their favorite TV channels.
How can this be? You had always been taught that ventricular fibrillation is not just a "life-threatening" rhythm but rather a bona-fide "lethal" rhythm 100% of the time. What kind of voodoo black magic is at work here? This patient should be dead or, at the very least, gorked out and in their death throes. You dare not initiate CPR as it is contraindicated here. The code team has already been activated but there is little for them to do as they file into the room one-by-one. As you quickly evaluate the patient, you find them to be A&Ox4, pulse = 70/min, BP = 120/80, and all other vital signs are within normal limits.
In the heat of the moment, one nurse has the mental fortitude to verify that the patient is correctly matched up with the right piece of equipment (i.e., the telemetry monitor box) and this is confirmed to be the case. A mix-up of equipment might mean that another patient, at a remote location, is actually the one who is in V-fib and is coding elsewhere on the ward. In the past, this has also happened!
This is the very definition of "an enigma wrapped in a paradox": The rhythm is unequivocally verified to be V-fib however the patient is asymptomatic and has no chief complaint.
- Question: Under what circumstances can a patient's rhythm be in V-fib and yet they are able to maintain consciousness, a pulse, and a blood pressure?
I had a clinical nurse specialist pose this very question to me about a decade ago. Being the "seasoned" telemetry technician that I was, I naturally said that there was no way that a patient could be in V-fib and be among the living at the same time. How wrong I was. She told me that this real-life scenario actually played out at the hospital we were both working in at that time and I've even seen a similar case published in one of the textbooks I own in my personal library.
Source / Reference:
1.) Rimmerman CM, Jain AK. Interactive Electrocardiography: CD-ROM With Workbook. 1st ed.
Philadelphia, PA: Lippincott Williams & Wilkins; 2001. p. 209
Please share your comments.
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
ANSWER: If the patient is in
ANSWER: If the patient is in a Cath lab where the team noted the precise onset of this rhythm - and instructed the patient to then cough forcefully and repetitively (has been shown to work, at least for up to 90 seconds - by which time presumably their VFib can be definitively treated ... ).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
response
Patient that has a VAD or TAH??
Christine Schaeffer
LVAD
A patient with an LVAD may be in V-Fib... the LVAD may still produce perfusing pressure while this dysrhythmia is occuring.
VADs: Only thing keeping some patients alive!
If you were thinking that the answer to my question is VLAD (as in “. . . the Impaler”), then you are incorrect. The right answer is LVAD. Traditionally, a Left Ventricular Assist Device, which is better known (in the interest of brevity) by its acronym LVAD (pronounced “EL-vad”), has been considered a “bridge” device. The hope was generally that it would keep the patient alive long enough to eventually receive an orthotopic heart transplant. A Biventricular Assist Device (BIVAD) can also compensate for V-fib by generating a viable pulse and perfusing blood pressure as DaveB indicated.
A Right Ventricular Assist Device (RVAD) alone will not be adequate enough to keep you alive in the setting of V-fib. Of the 4 chambers of the heart, the left ventricle (LV) is affectionately considered the “workhorse” and a LVAD is literally “assisting” the LV just as its descriptive name is suggesting.
When I would teach new students about how to recognize V-fib (and V-Tach for that matter), I would always include this scenario as part of my curriculum.
Please indulge my “War Story”: Many years ago when I was employed full-time on night shift as a Cardiac Monitor Technician (CMT), I was remotely monitoring a patient on a different unit and that patient suddenly converted from normal sinus rhythm into a monomorphic ventricular tachycardia (MMVT) at a rate well in excess of 200/min. As per protocol, I promptly notified the patient’s nurse via telephone and she informed me that the patient had an LVAD and she was not going to check on him but rather she was content to just let him sleep on through the remainder of the night. This patient did not have an implantable cardioverter defibrillator (ICD). What may have been a code-blue for any other person did not even warrant evaluating the patient in this instance. He was in sustained MMVT for 5+ hours and slept like a baby through the whole thing, never the wiser of my concerns. Reluctantly, I had to completely suspend all of his alarms because they were chronically drowning out other alarms and preventing me from safely monitoring the other patients on telemetry.
Key point: Always assume that V-fib is a 100% lethal rhythm, but don’t be surprised if it turns out the staff are not “coding” an LVAD or BIVAD patient.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]
norma
suspend all of his alarms because they were chronically drowning out other alarms and preventing me from safely monitoring the other patients on telemetry. wrdshan