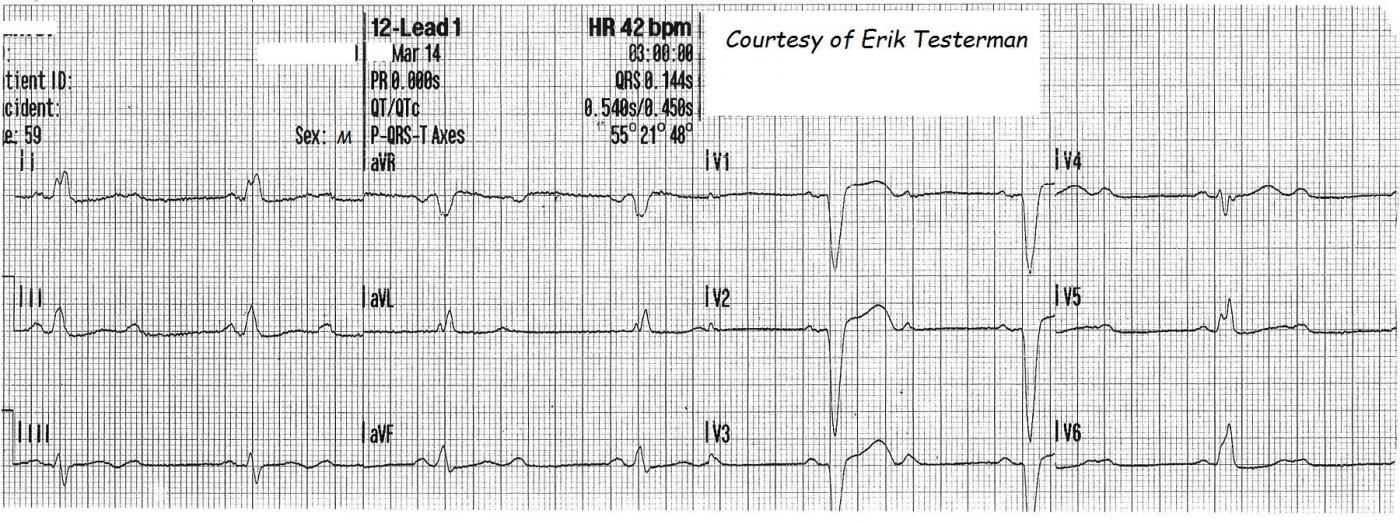
Paramedic Erik Testerman has generously donated several excellent teaching ECGs to the Guru, and we will be featuring all of them soon. This week, we show you the ECGs from a 59-year-old man with a blood glucose of 30 mg/dl. He had no complaints . After a bolus of Dextrose 10%, his blood glucose was 105 mg/dl. He gave a past medical history of diabetes mellitus, hypertension, and left bundle branch block. Vitals were reported as normal and stable, except for the slow heart rate.
The first ECG, taken in the field, show a second-degree AV Block. The conduction ratio is 2:1. That is, there are two P waves for every QRS complex. With this ratio, it is sometimes difficult to determine whether the patient has Type I (usually AV nodal) or Type II (Infranodal) AVB. In order to diagnose Type I AVB (Wenckebach), we need to see TWO P waves in a row conducted, to see the prolongation of the PR interval. It is not correct, however, to call ALL 2:1 AV blocks "Type II". Often, simply taking a longer rhythm strip will expose a period of 3:2 conduction, showing progressive prolongation of the PRI.
This ECG, however, gives us some clues that it is probably TYPE II. The patient has a left bundle branch block. Type II AVBs are infranodal - that is, they affect the structures below the AV node: the His Bundle and the Bundle Branches. Type II AVBs represent INTERMITTENT TRI-FASCICULAR BLOCK, and that is common in the presence of RBBB and LBBB (a bi-fascicular block). This ECG probably represents an existing LBBB with an intermittent RBBB - When the right bundle is blocked, the patient has a tri-fascicular block, and no conduction to the ventricles.
Another clue that this is Type II is that the NON-CONDUCTED P waves fall CLEAR of the preceding T waves, meaning that they had ample opportunity to conduct, not being in the absolute refractory period.
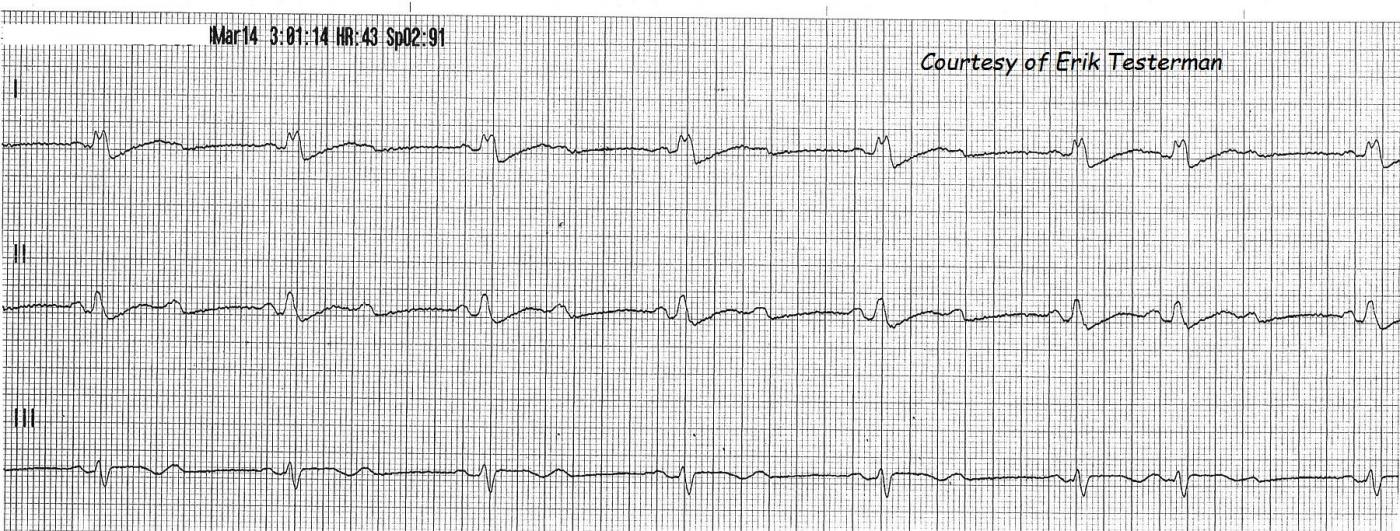
Fortunately, the rhythm strip, taken one minute later, uncovers the diagnosis! The sixth and seventh QRS complexes are conducted with a 3:2 ratio, showing PR intervals that stay the same, proving the rhythm is Type II.
For this patient, the heart block and resulting bradycardia don't seem to be causing symptoms. But infranodal blocks can easily progress to complete heart block and should be treated with implanted pacemakers. The EMS crew in this case had transcutaneous pacer pads on the patient as a precaution, but he remained well-perfused and with a good BP the whole time.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Mobitz I vs Mobitz II
For reinforcement of these concepts regarding the various Types of 2nd Degree AV Block - and distinction between Mobitz I vs Mobitz II - Please check out these 3 ECG Blogs:
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Dawn and Dr. Grauer, I thank
Dawn and Dr. Grauer, I thank you so very much in expanding on this case I donated. I love everything about being a Paramedic, but I mostly love Cardiology!!! Further info on this pt, when I arrived at the hospital, his pulse was resting around 30 bpm, still in the 2:1 AV Block. The charge nurse unfortunately did not take me very seriously, and I was given a weird look as to why I had pacer pads on him.
Any words of advice either of you two may have for me to better myself would be greatly appreciated!!
Erik Testerman, AAS, LP, NREMT-P
Thanks, Erik
You don't really need my advice! You are obviously a Paramedic who cares about doing a good job for your patients, and that is what matters. In order to do this, you have to keep studying (you are doing that) and you have to follow up on your calls to learn as much as possible from them (you are doing that). Thanks so much for sharing your ECGs with the ECG Guru so that others can learn, too.
Dawn Altman, Admin