Submitted by jer5150 on Sat, 01/26/2013 - 15:48
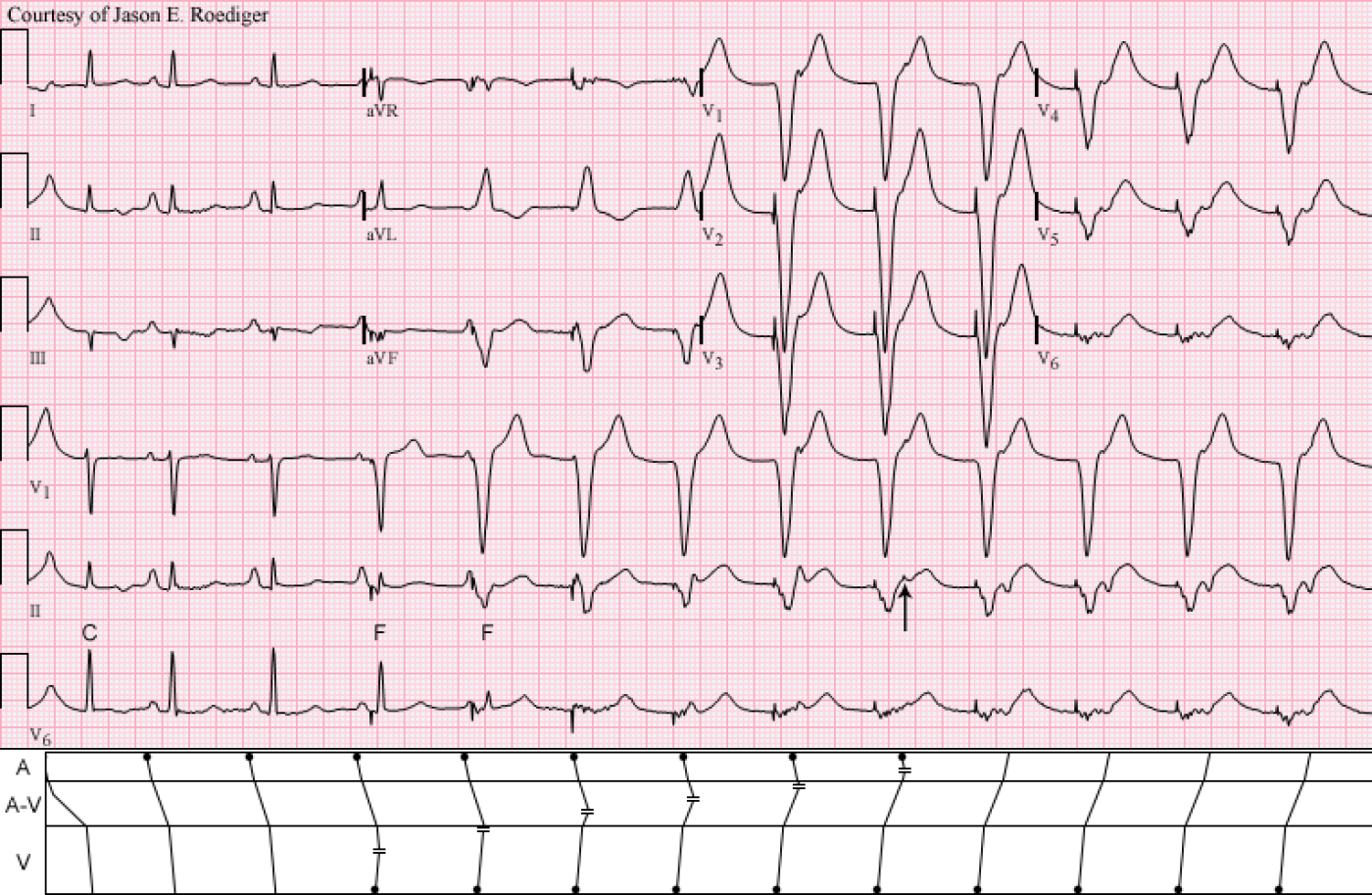
Patient's clinical data: 67-year-old white man with a history of COPD and CAD.
Unfortunately, due to the advanced age of this ECG (29-years ago), many details of the device will have to be left to speculation. I'm unable to retrieve any information about the patient other than the two diagnoses above.
How many different things can you spot in this 12-lead ECG?
Rate this content:
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
This is a nice ECG!
The frist P wave is seen on the top of the T wave. The morphology of the T wave is different from the two other T waves morphologies [the native and the paced] in the strip rhythm. This first P wave is conducted with long PR compared to the following normally conducted P waves, this suggests dual AV node physiology. The first 3 QRS complexes are of the same morphology and they are normally conducted. The fourth to the 6th QRS complexes are fused beats. Then the pacemaker takes over and the QRS complexes are pure paced. The last four beats have retrograde P wave [VA conduction]. Few comments about the pacemaker: The paced rhythm is ventricular only, therefore the device is a single chamber. The paced beats morphology suggestive of RV apical pacing, which means either it is a transvenous temporary or permenant pacemaker. Now the one million dollar question: why the pacemaker started pacing???? The simplest answer is give me the pacemaker parameters. Anyway, if we look at the heart rate it is about 85 bpm, this suggests either it is a permenant pacemaker and the magnet just placed on the device, or the pacemaker is a temporary and someone increased the rate to 85. This is definitely VOO pacing or unlikely undersening!!! Looking forward to hearing your answer.
Agree - Nice ECG with Lots of Findings!
I see the following on this ECG:
1) Underlying sinus rhythm
2) RAE (tall, peaked P wave in lead II )
3) Inferior ST flattening, T inverted in III - possible ischemia
4) Paced rhythm - sensing & capturing appropriately (assuming fixed rate of 80/minute which is quite fast is intentional); Pacing begins with beat #4 as sinus rate slows slightly ...
5) Fusion beat (beats #4,5)
6) Retrograde conduction after paced beats
7) Concealed conduction - Can't tell if there was a PVC just before this tracing began - with P wave on the T (right after the standardization mark) - with this P wave conducting with a long PR (due to concealed conduction).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
?AV dissociation
Rather than retrograde VA conduction, I think there may be AV dissociation with sinus P waves throughout. The PP intervals seem constant and the P waves appear to march through the paced QRS and out the other side with an increasing RP interval.
Dave R
Rate-Responsive?
And maybe this pacemaker, firing in VVI mode, also has a rate-responsive feature which was just triggered to start pacing at a rate slightly faster than the sinus rate?
Walter A. Mueller, CCT, CRAT
Why not Rate Response. . .
If it was rate response, then it should be in VVI[R] mode and not VOO mode, therefore, there should be sensing of the QRS and you do not see fusion beats.
Pacemaker Fusion
I've always been under the impression that pacemaker fusion and pseudo-fusion can occur with any ventricular pacemaker regardless of programming mode and that you can't definitively call it failure to sense unless the ventricular pacer spike occurs at the very end of, or after the QRS complex. Up until then it may just be a matter of timing with the pacemaker firing just before the natural ventricular activation reaches the site of the pacer electrode.
Walter A. Mueller, CCT, CRAT
Fusion and pseudo-fusion
That is true if the patient had RBBB, then the LV will be activated earlier and the sensing will be delayed because the pace-sense bipole is located in the RV apex. In this case, the QRS morphology is normal. Remember, sensing in the pacemaker is set to 2.5 mV and the sensed R wave usually > 5 mV, therefore, the sensing occurs in the first 40 ms of the QRS and you do not need to wait until the end of the QRS to see the fusion and pseudo-fusion.
VVI or VOO?
Firstly, I take back my previous comment sbout AV dissociation. I wasn't displaying the ECG correctly and didn't see the last few beats with obvious retrograde conduction.
I can't see any non-sensing of intrinsic QRS complexes, so I'm not sure that it's possible to state whether this is VVI with an unusually high pacing rate or VOO, perhaps caused by a magnet being placed over a Medtronic pacemaker. I'm looking forward to Jason's explanation!
Dave R
Thanks
Thanks Jason. Nice case. I agree - likely VVI pacing (probably non-rate responsive temporary lead pacing). Progressive QRS fusion as the sinus rate drops below the fixed rate of the pacemaker. Retrograde P waves seen after the last few beats. The first P wave's (seen on the first T wave) conduction through the AV node is delayed due to a partially refractory AV node (atrial impulse falls within the relative refractory period of the AV node) - likely caused by a retrograde conduction from a previous paced beat (concealed conduction). Q waves can be seen in the intrinsically conducted beats in leads III, AvF which suggest a possible previous inferior infarction - this may have been the reason for placement of the temporary pacemaker lead in the first place.
www.heartrhythm.co.za
Follow me on Twitter @heartrhythmcoza
Correction
I have made a correction to my post above (already edited). I meant "sinus rate dropped below paced rate", not "sinus rate EXCEEDED paced rate", as originally stated.
www.heartrhythm.co.za
Follow me on Twitter @heartrhythmcoza
INTERPRETATION
Let me reiterate that this ECG is 29-years old and I know virtually nothing specific about this case. It is chock-full-o' interesting findings though so this is my official read on what's happening here.
I’m not going to count it as a true “beat” because it is only partially-inscribed, but the first waveform is presumably the T-wave of a ventricularly paced beat with a sinus P-wave perched up on top of it's apex. This gives the T-wave a taller and sharper appearance. The next fully-inscribed beat (i.e., 1st beat) is presumably a conducted sinus beat which would probably be more correctly labeled as a ventricular capture (C) beat. This first beat is conducted with a prolonged P-R interval of 0.33s. I agree with both doctors (Raed and Ken) that this could be the result of either retrograde concealed conduction from a ventricular paced beat into the A-V node leaving it somewhat refractory OR that the ventricular paced beat could have conducted retrogradely into the fast pathway (FP) causing descending A-V conduction to “jump” over to the slow pathway (SP) for just the one sinus beat. In the laddergram, I have chosen to illustrate the mechanism as retrograde concealed conduction. The sinus rate is slightly irregular producing the following sinus cycles: 1st = 78/min; 2nd = 79/min; 3rd and 4th = 75/min; 5th – 8th cycles = 74/min. The 2nd and 3rd beats are conducted sinus beats with normal P-R intervals of about 0.16s. I agree with Ruan that the inferior q-waves in III and aVF could be suggestive of a previous inferior infarction.
When the sinus rate slows to 75/min, the pacemaker starts to pace the ventricles at a faster rate of 80/min. The 4th and 5th beats are paced fusion (F) beats with varying degrees of ventricular fusion. Beats 6, 7, and 8 are 100% ventricular paced beats that are dissociated from sinus impulses. In lead V1, the polarity of the QRS complex is wholly negative indicting that this is probably pacing the apex of the right ventricle (RV). Since there is no consensus between the two resident pacemaker experts (Raed and Ruan), I will just say that this is programmed to either VVI or VOO mode. Note, in the A-V tier, that I’ve illustrated an advancing retrograde wavefront as the anterograde wavefront progressively retreats backwards to the atria.
There was no mention of the atrial fusion (arrow) on the 9th beat. There are only two different types of fusion and they both occur on this ECG (i.e., ventricular and atrial). Electrocardiographically speaking, I don’t think the word “fusion” should ever be broadly used to describe situations where unrelated waveforms overlap one another. Case and point: At the beginning of this tracing, there is a simultaneous P-waves and T-waves. Some authors would refer to this as T/P fusion. A sinus P-wave represents atrial depolarization while a T-wave represents ventricular repolarization. These are two entirely separate events that are taking place on two different anatomic levels of the heart (i.e., upper and lower chambers). True fusion takes place in the same chamber as I've illustrated on the laddergram. That kind of misuse of the word “fusion” is only going to needlessly complicate and confuse those who are trying to learn about both atrial and ventricular fusion. I'm referencing this recently released video by a website that I otherwise respect: http://www.ecgteacher.com/index.php/arrhythmias/tachycardia-svt-1 If we were to accept this alternate definition of fusion, then common rhythms like atrial fibrillation are displaying fusion every time a fibrillatory wave coincides with a QRS complex or T-wave.
Beats 10, 11, 12, and 13 are ventricular paced beats with 1:1 retrograde ventriculoatrial (V-A) conduction to the atria. Note in the laddergram that V-A conduction is comparable to atrioventricular (A-V) conduction. Since the R-P’ interval (0.19s) on the ventricular paced beats is comparable to the P-R interval (0.16s) on the sinus beats, one can infer that V-A conduction is taking place over the A-V node’s fast pathway (FP). If Raed is correct in assuming that the capture beat conducts anterogradely over the SP, then retrograde conduction over the SP would certainly produce an R-P’ interval in excess of 0.33s.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]