All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.
Recent blog posts
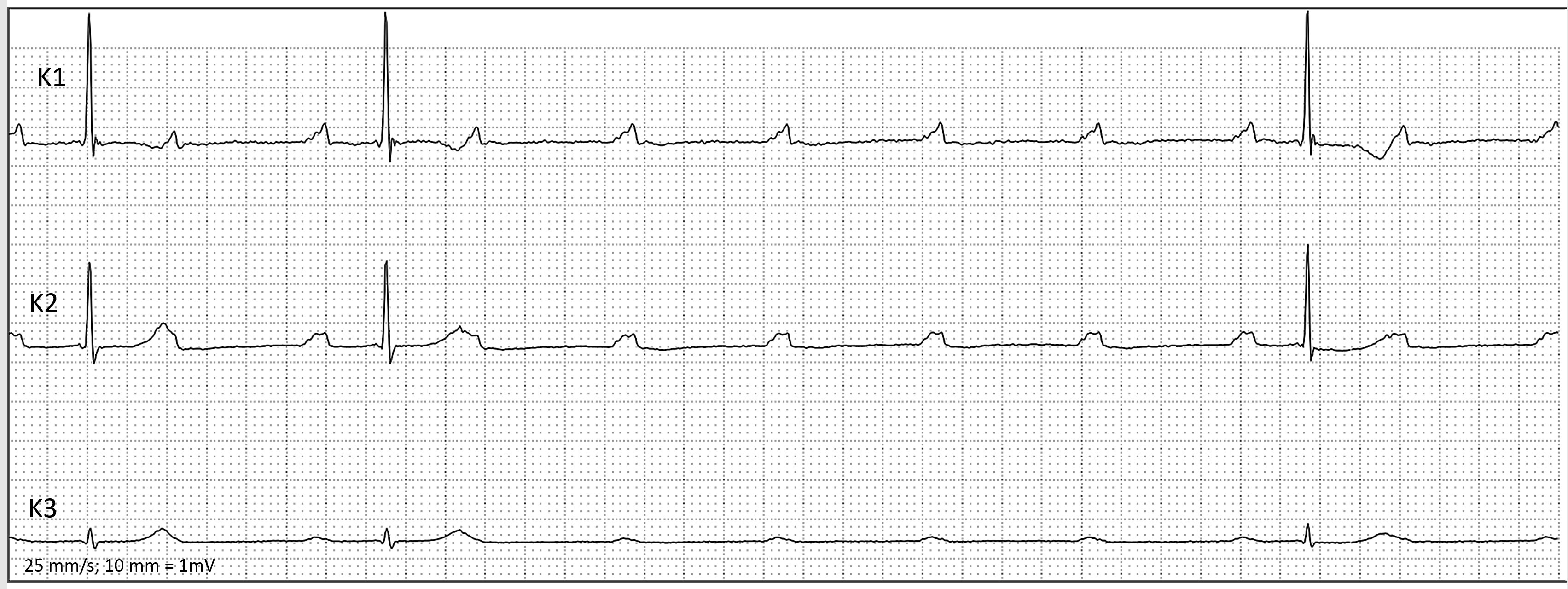
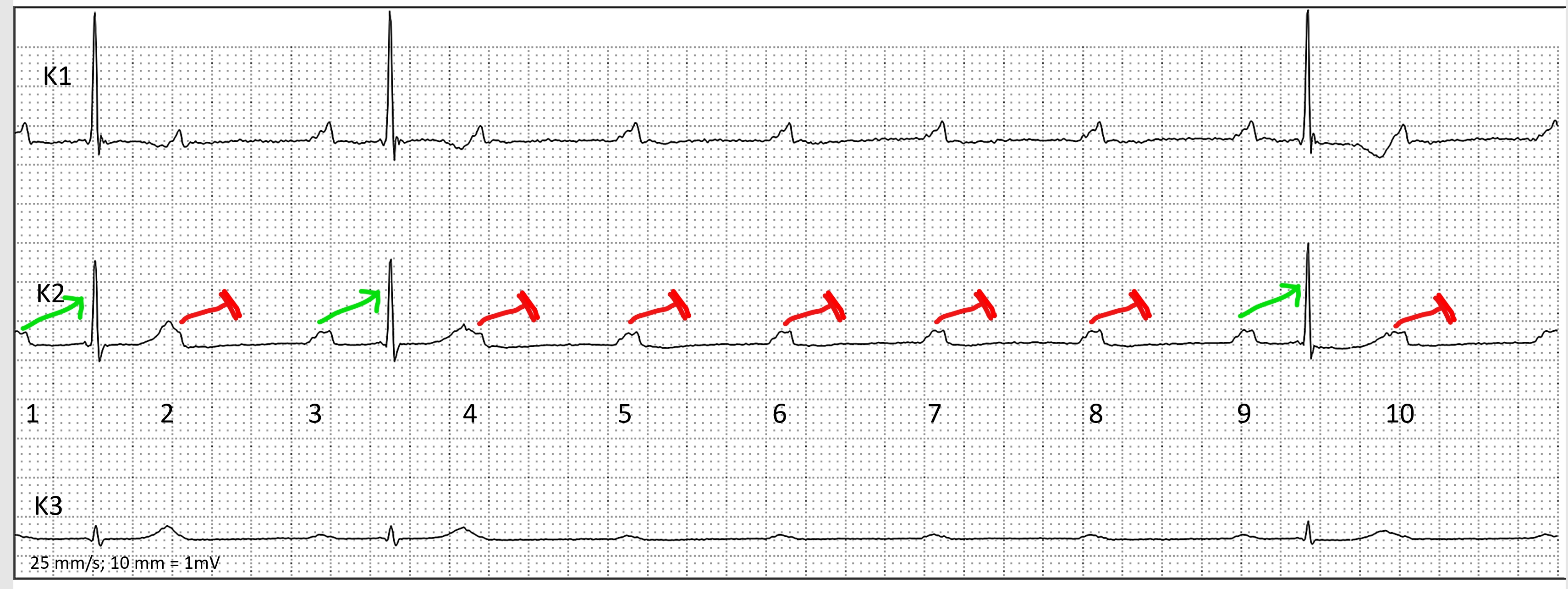
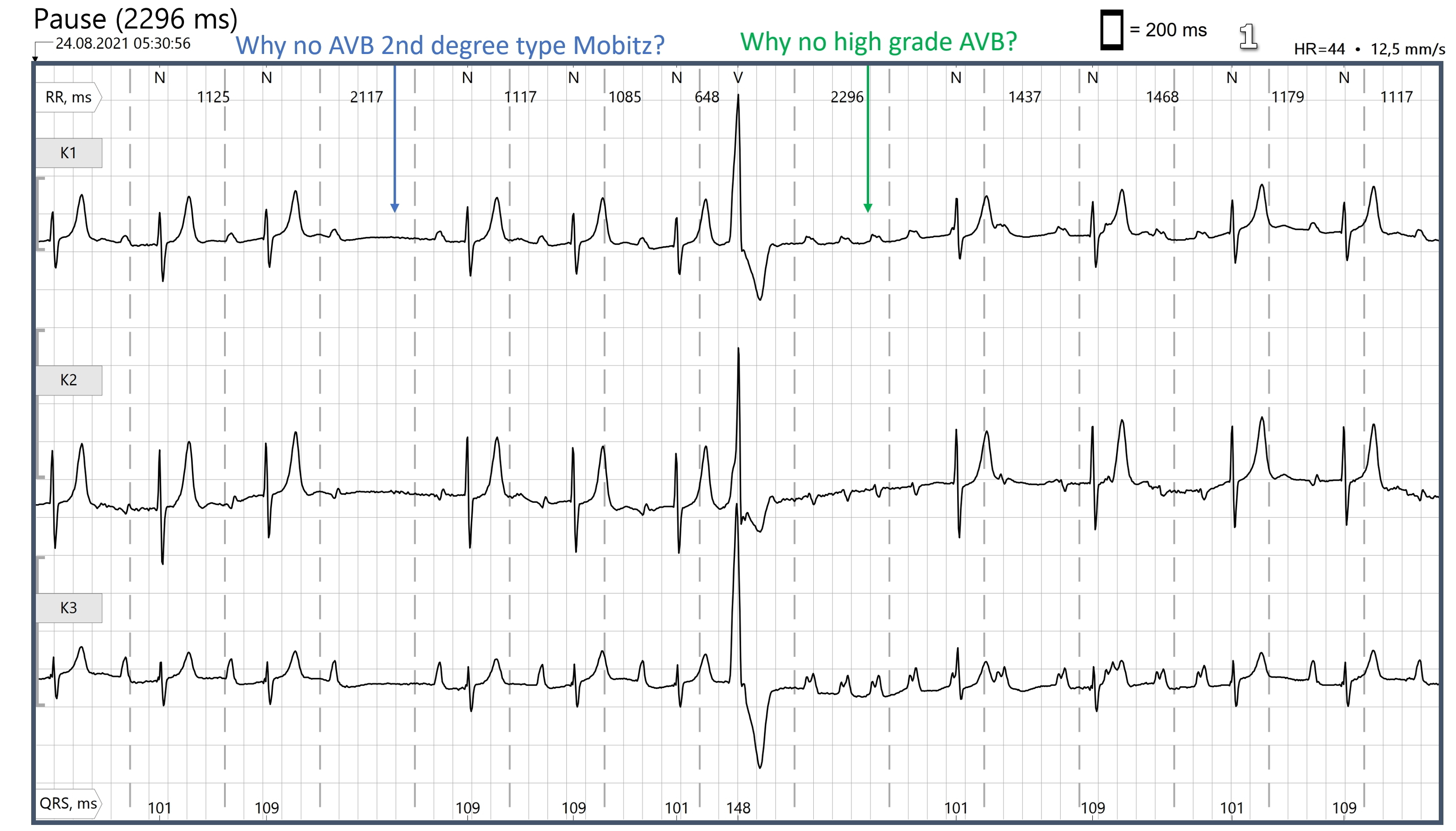
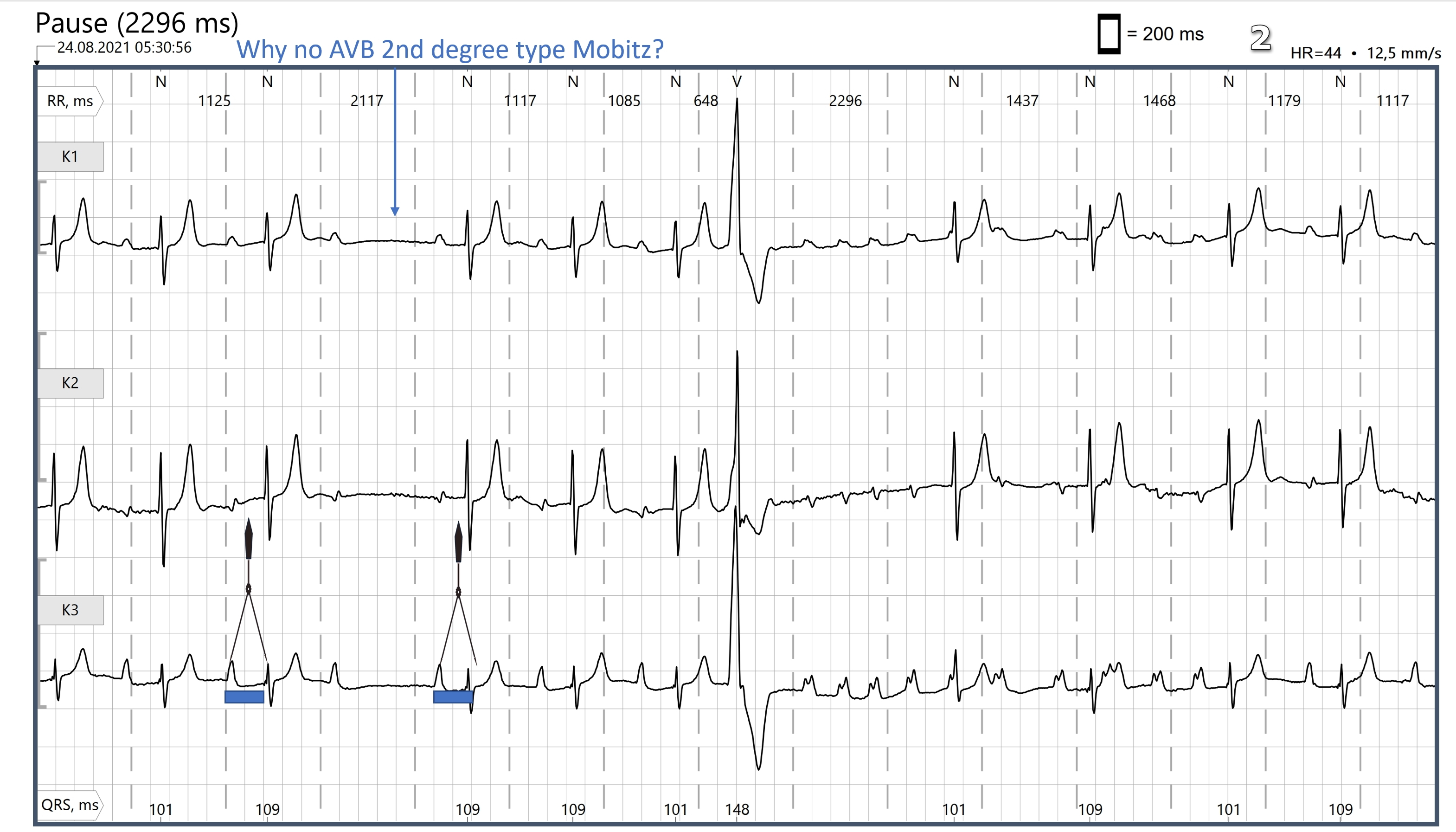
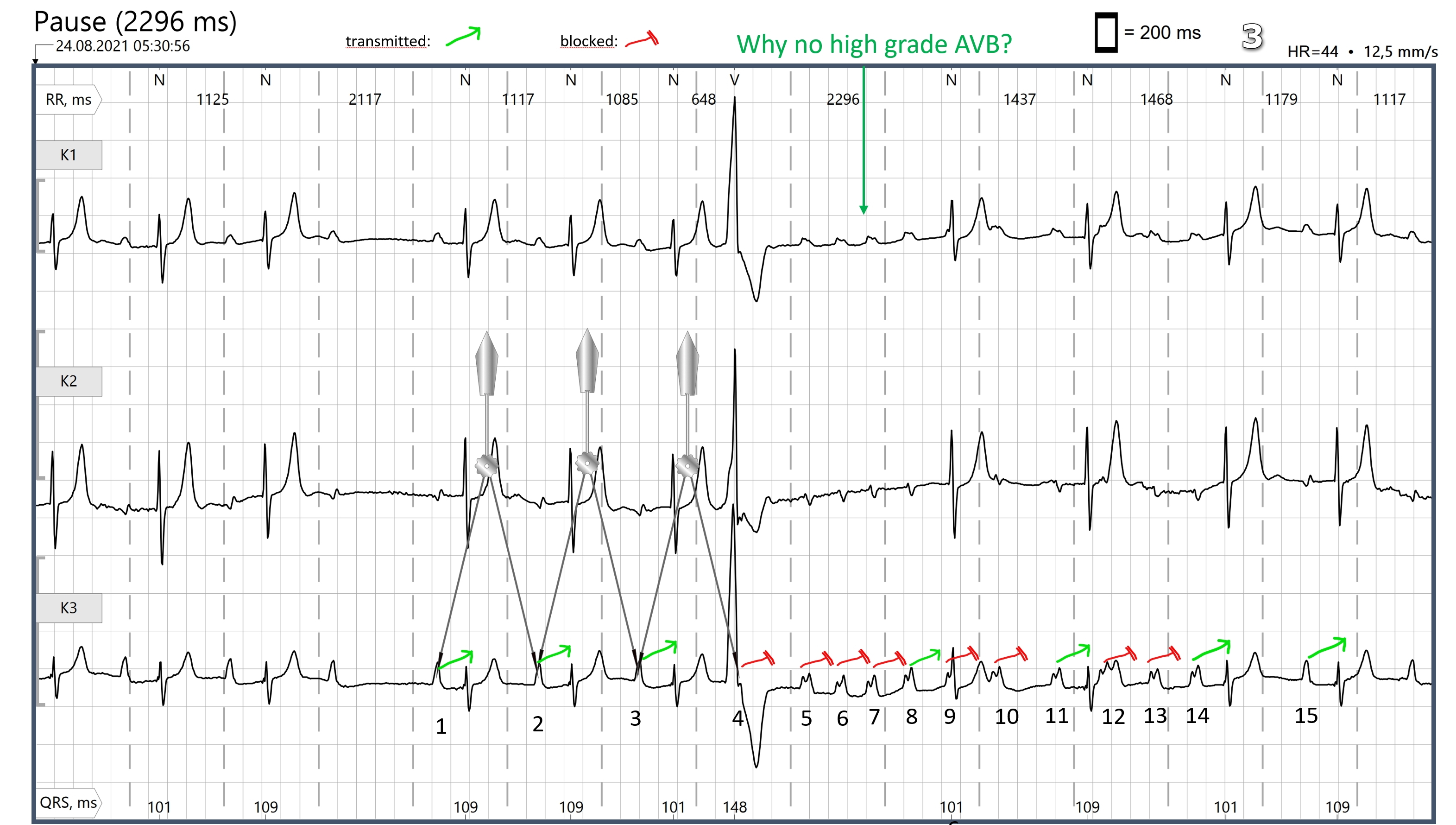
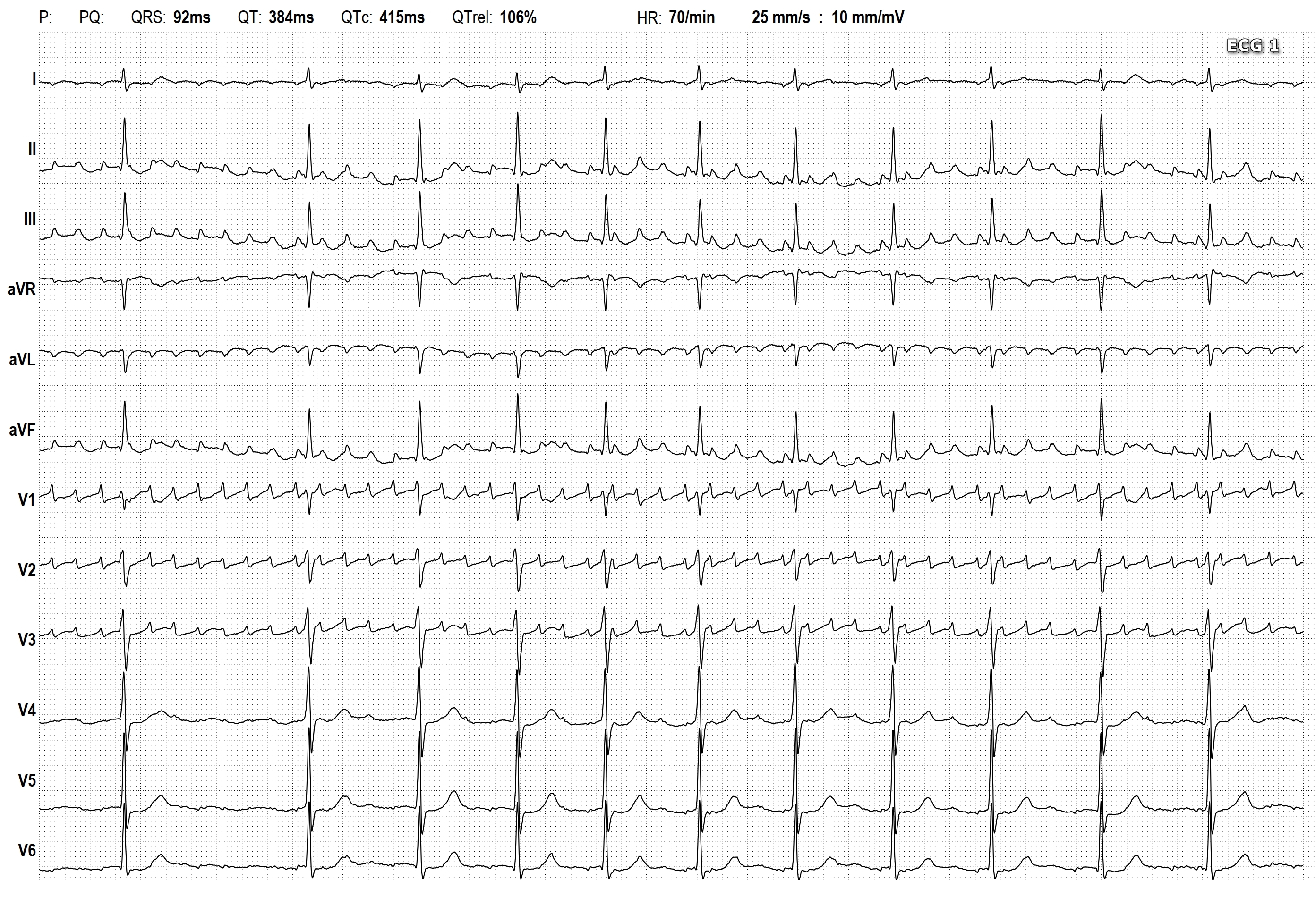
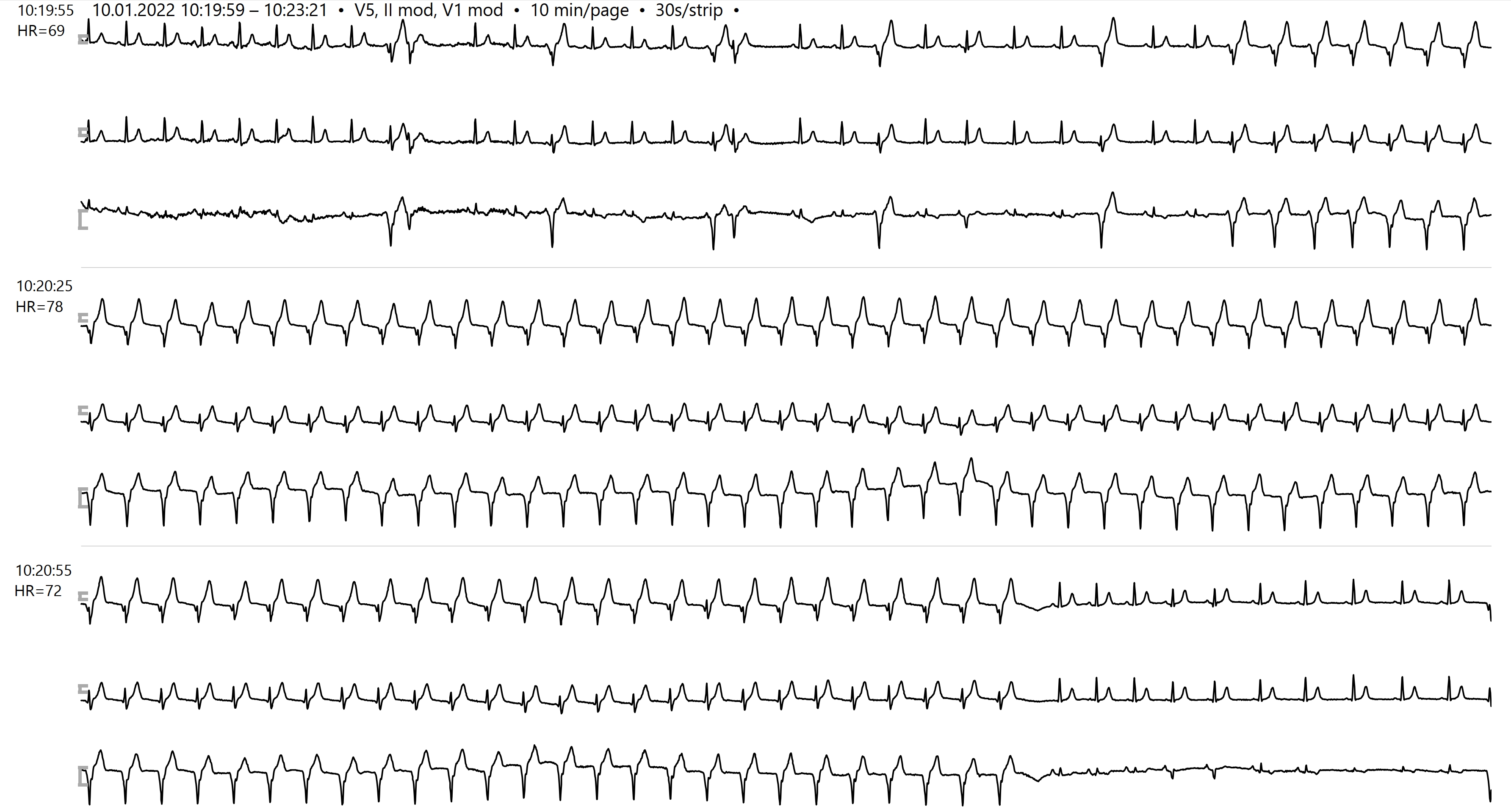
- An Interesting Holter Strip
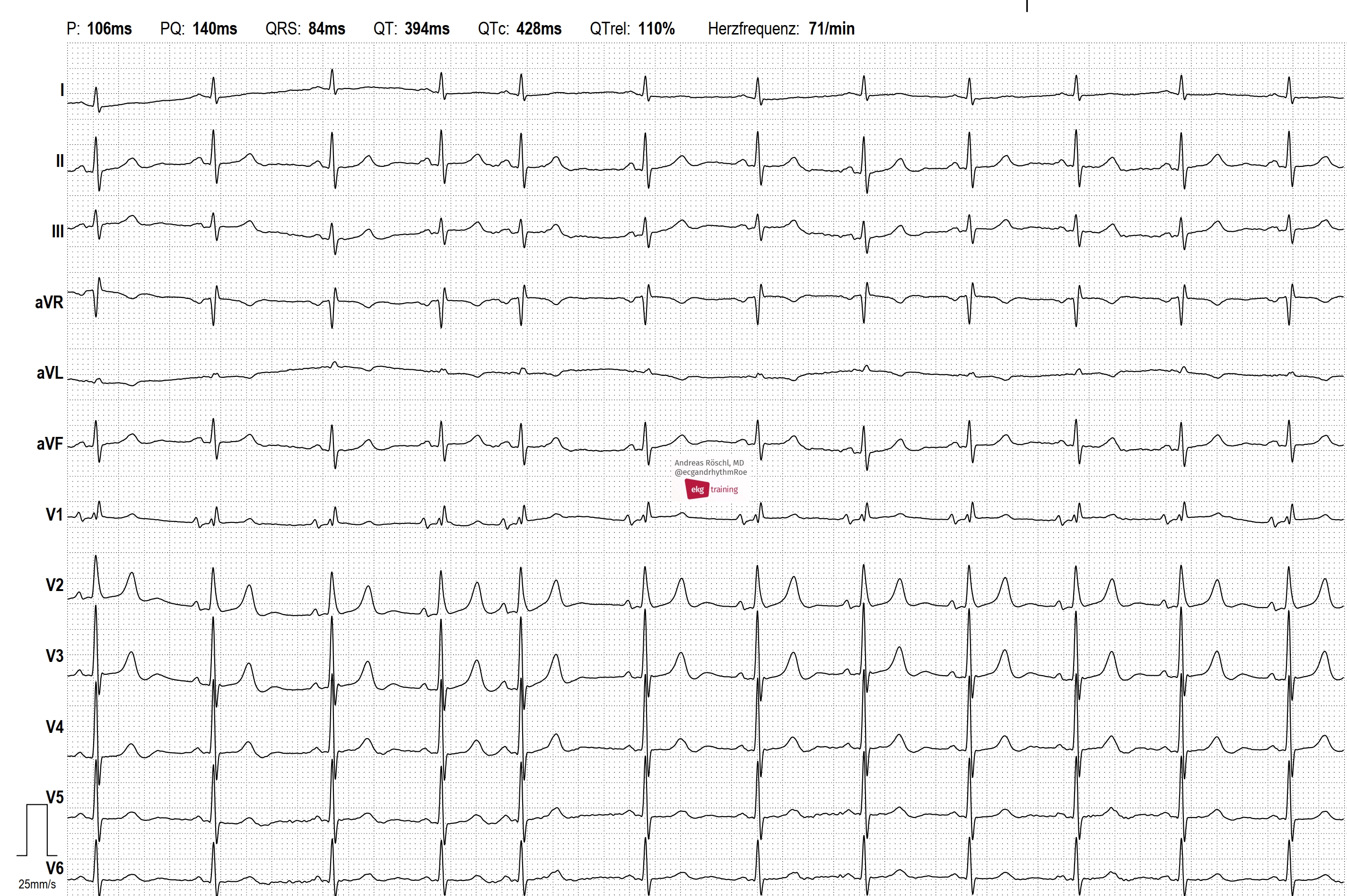
- Atrial Fibrillation With Rate-related Left Bundle Branch Block
- New Book From Dr. Jerry Jones
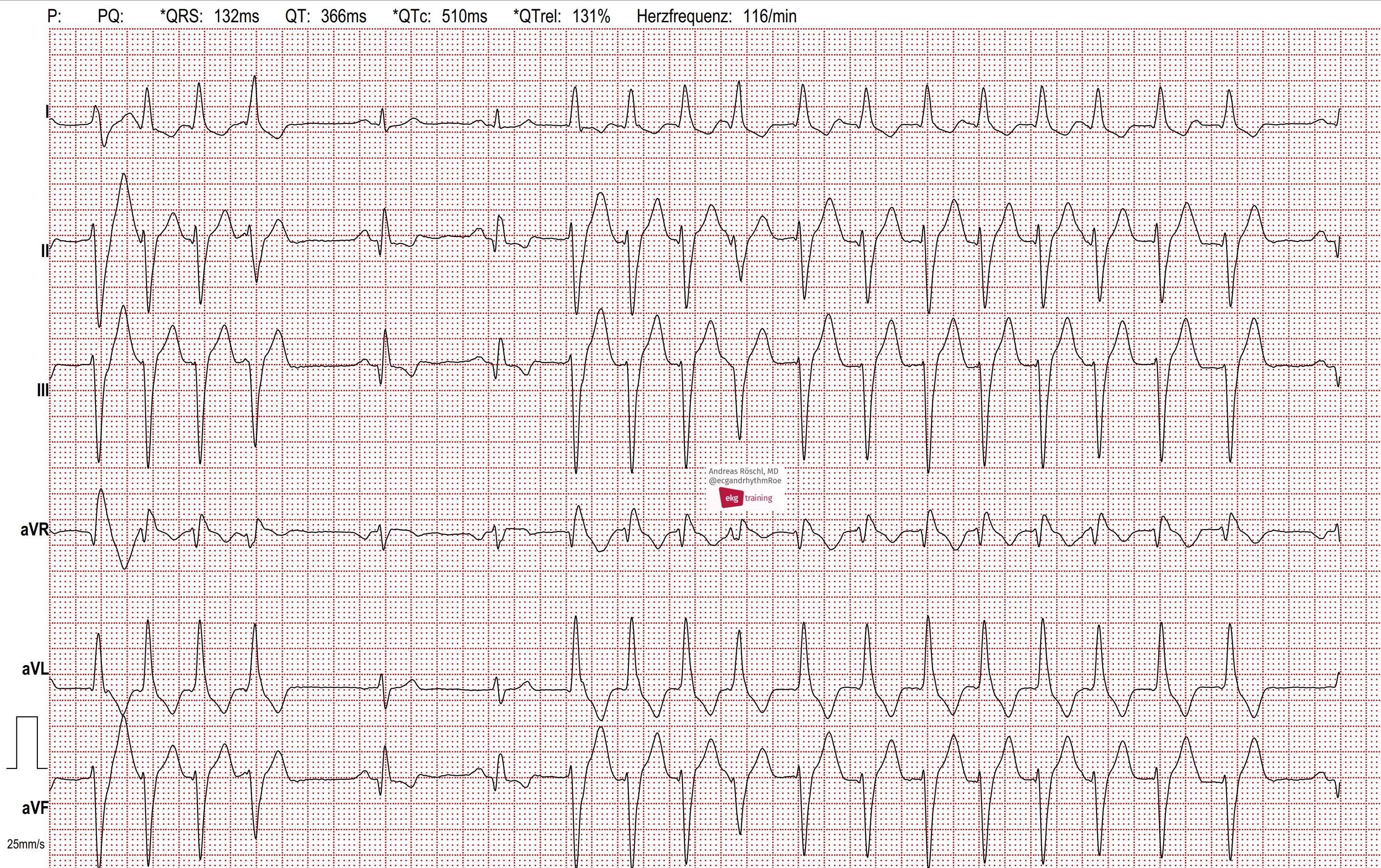
- VENTRICULAR TACHYCARDIA WITH SUCCESSFUL ATP
- SUSTAINED VENTRICULAR TACHYCARDIA
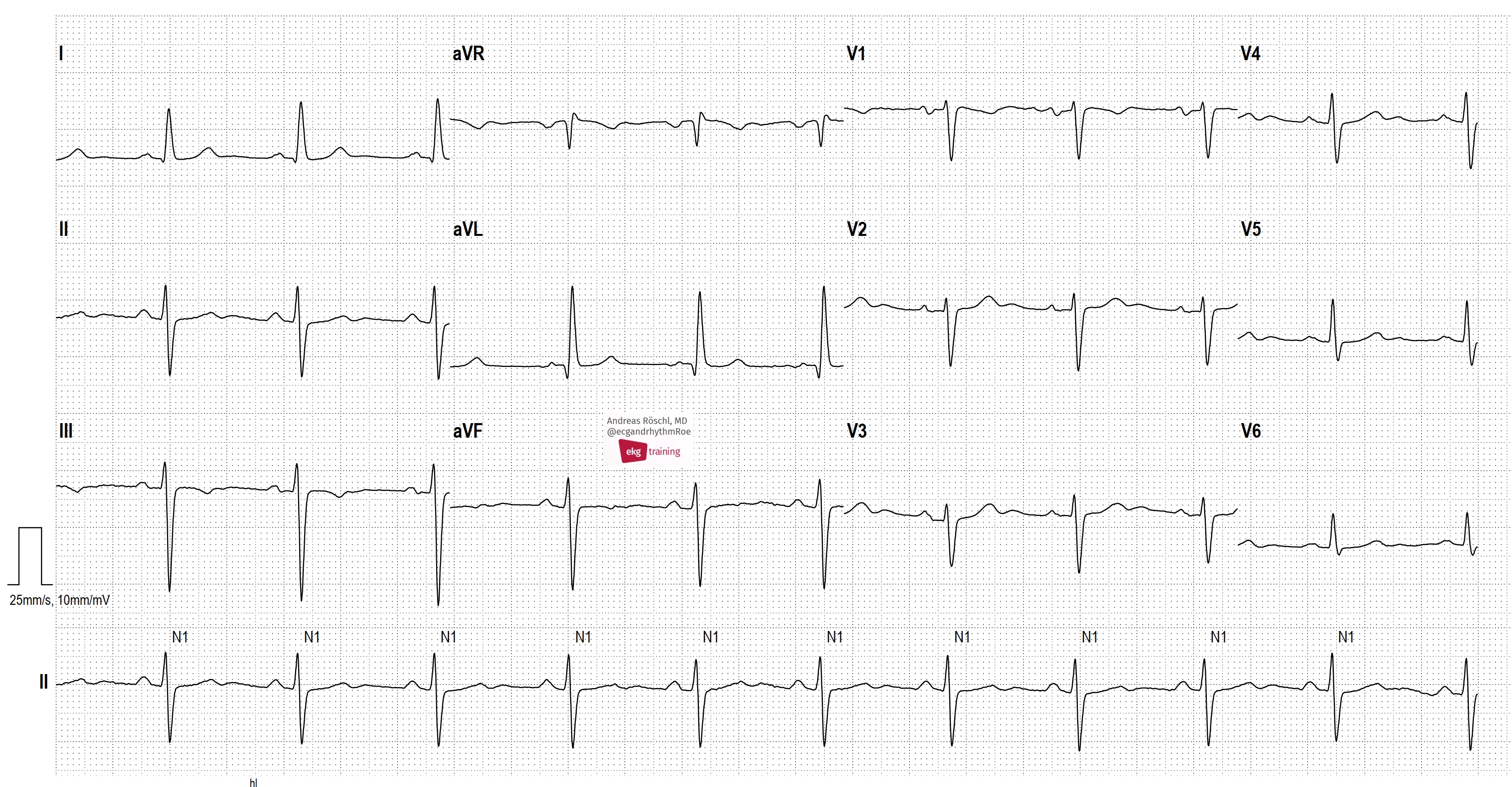
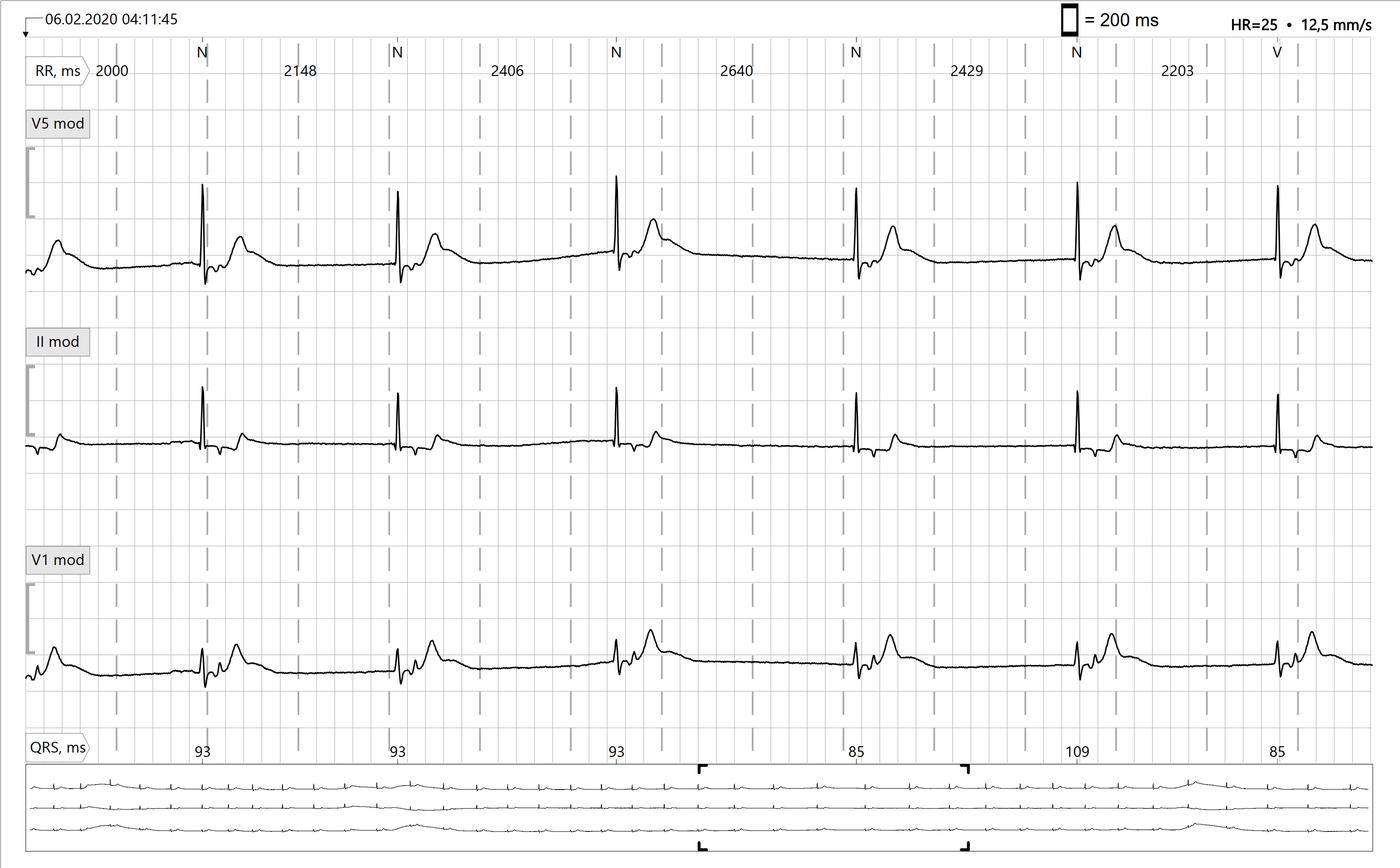
- SICK SINUS SYNDROME
- Atrial Flutter With Right Bundle Branch Block and Left Anterior Fascicular Block In a Patient With Preexisting RBBB + LAFB
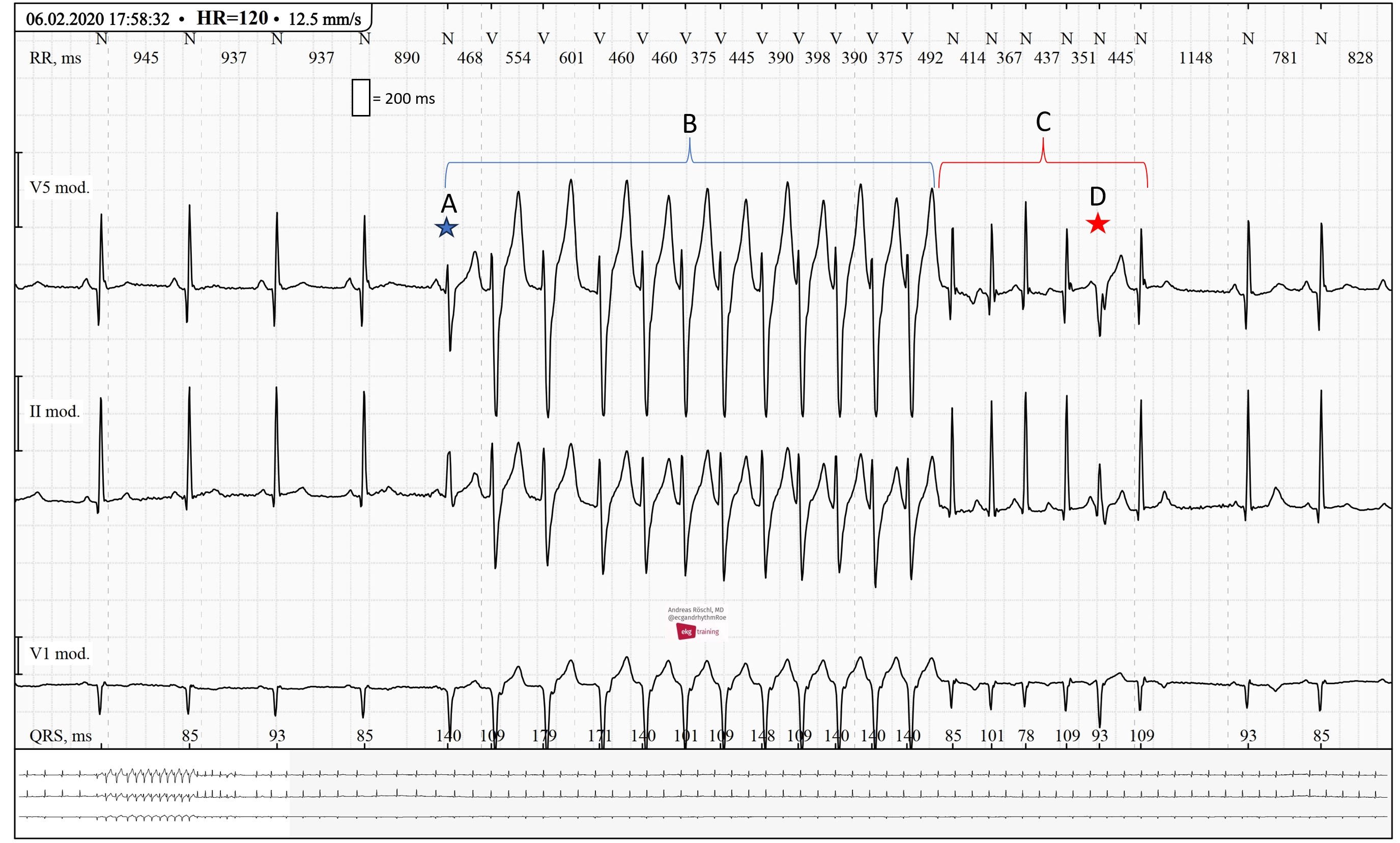
- Ventricular Tachycardia. Unsuccessful Antitachycardia Pacing in an ICD Patient
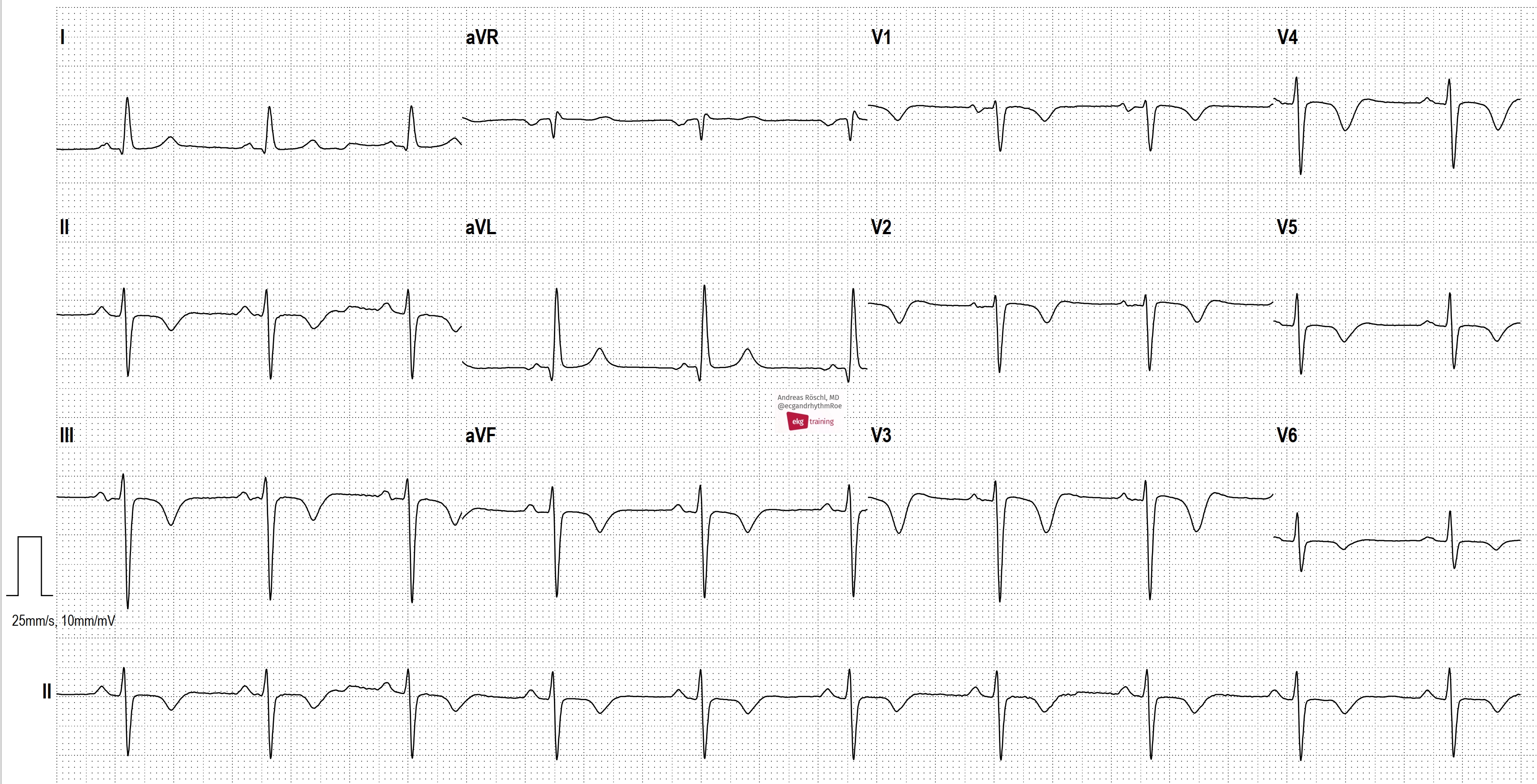
- High-grade AV Block
- Atrial Flutter Degenerates Into Atrial Fibrillation
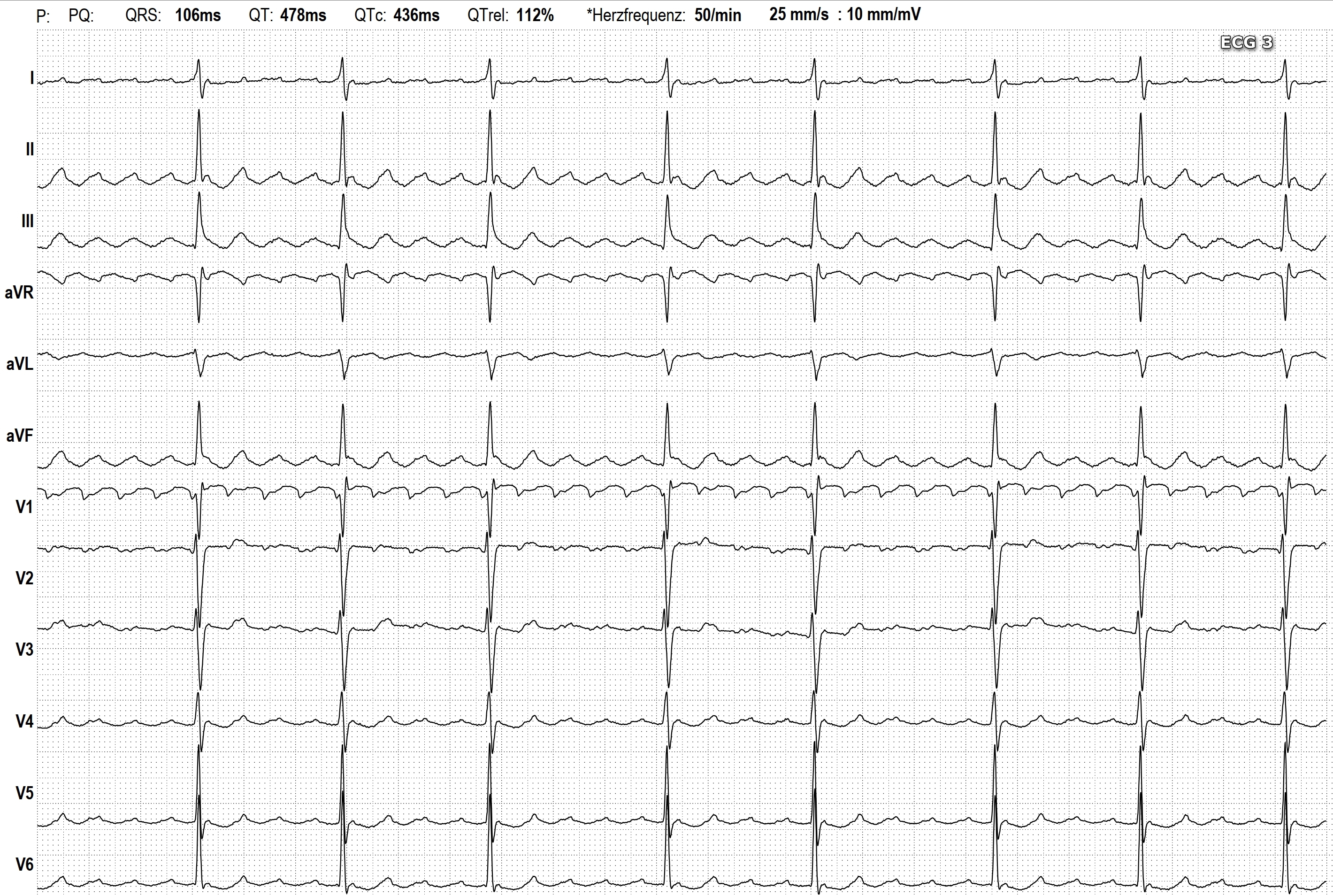
- Sinus Bradycardia and More
- SMART WATCH ECG
- Atypical Atrial Flutter (From the Left Atrium)
- Ventricular Tachycardia
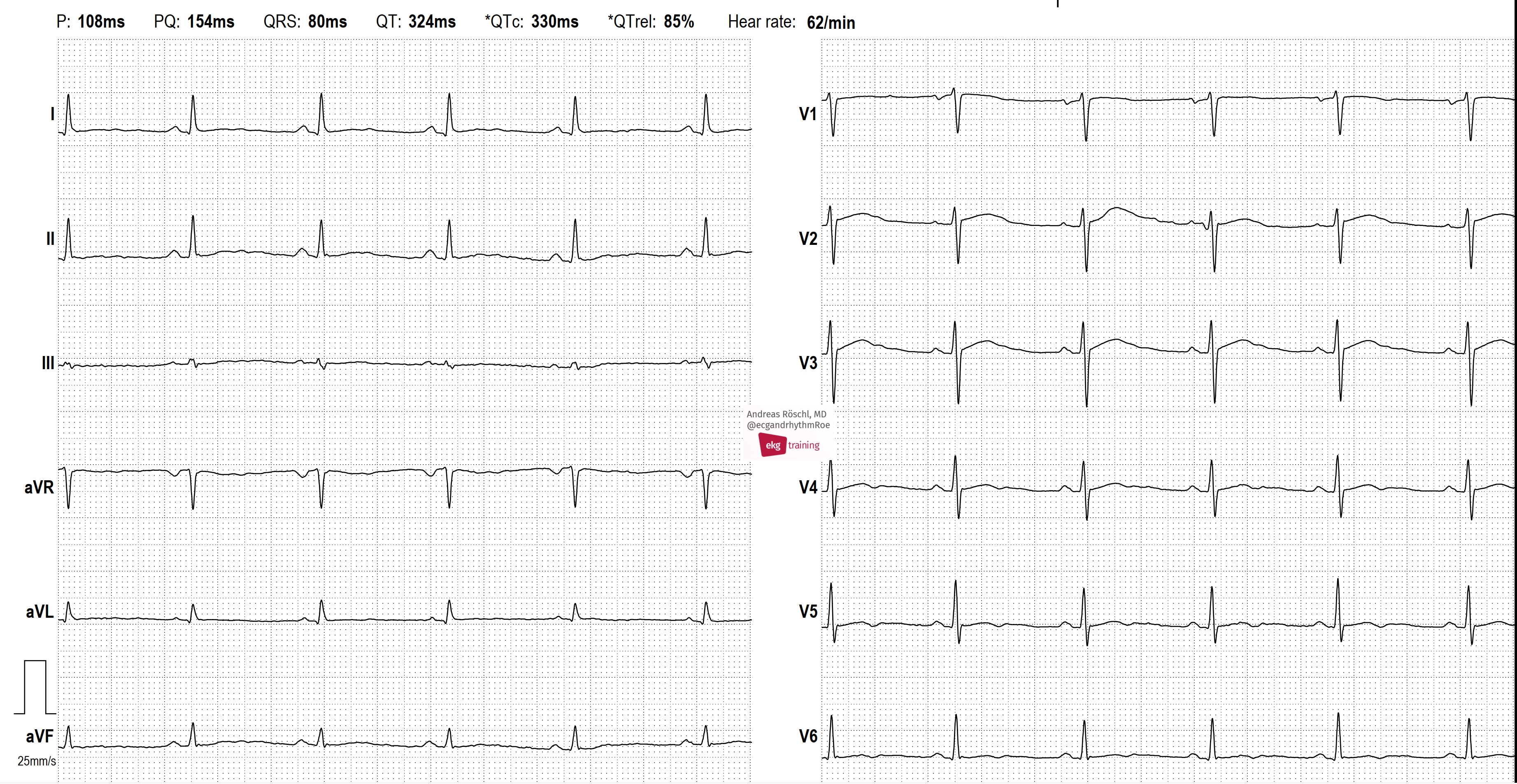
- Right Bundle Branch Block